Small Intestine: Bowel Resection & Anastomosis
Bowel Resection
Principles
- Ensure Good Blood Supply – Judge Subjectively or Use Doppler/Scintigraphy
- Ensure Adequate Mobilization & Avoid Tension
- Angle Transection Line Straight or Somewhat Oblique to Keep Antimesenteric Edge Shorter & Ensure Good Blood Supply
Technique
- Classic Technique
- Place Non-Crushing Bowel Clamps on Both Sides of the Transection Line
- Sharply Transect the Bowel Using a Scalpel
- Repeat at the Opposite Bowel Margin
- Transect the Mesentery Using an Electrosurgical Device or by Clamping & Tying
- Linear Stapler Technique (More Common)
- Pinch & Thin the Mesentery Just Under the Site of Transection
- Make a Small Mesenteric Defect at the Site
- Insert One Jaw of the Stapler Through the Defect
- Assemble & Fire the Stapler at the Transection Line
- Repeat at the Opposite Bowel Margin
- Transect the Mesentery Using an Electrosurgical Device or by Clamping & Tying
Bowel Anastomosis
General Principles
- Strength Layer of Bowel: Submucosa
- All Layers Help
- Strongest – Esophagus Mucosa Squamous Cell Layer
- Center Side Reconstructions On:
- Small Bowel: Antimesenteric Border (High Risk for Ischemia if Elsewhere)
- Large Bowel: Taenia Coli (Adds Strength)
- Anastomosis Weakest Time Point: 3-5 Days (Breakdown Exceeds Production)
- Increased Collagenase Compared to Skin
Type of Anastomosis
- End-to-End
- The End of One Loop is Anastomosed to the End of Another Loop
- More Physiologic in Replication of Normal Gut Motility
- End-to-Side
- The End of One Loop is Anastomosed to the Side of Another Loop
- Considered When There is a Size Mismatch (Small Bowel to Colon) Although Others are Still Possible
- Side-to-Side
- Bowel Loops are Oriented Side-to-Side in an Overlapping Fashion
- Most Common when Using a Linear Stapler
- Types:
- Isoperistaltic: Ends are Approximated to Maintain Similar Directions of Peristalsis
- Technically More Difficult
- Antiperistaltic: Ends are Approximated with Opposite Directions of Peristalsis
- Technically Less Difficult
- Often Referred to as “Functional End-to-End”
- Isoperistaltic: Ends are Approximated to Maintain Similar Directions of Peristalsis
Method
- Hand-Sewn
- Excise Staple Lines if Present
- Use a Stay Suture to Approximate Both Bowel Ends
- Create Anastomosis with Full-Thickness Bites Using Absorbable Suture – Techniques are Varied (Interrupted vs Running/Direction of Travel)
- Consider Seromuscular Lembert Sutures to Buttress as a Second Layer
- Close the Mesenteric Defect
- Stapled
- Traditional Method:
- Resect Proximal & Distal Ends
- Sharply Excise the Antimesenteric Corner of the Resected Ends
- Place the Two Jaws of the Linear Stapler Through Each Opening
- Arrange the Jaws Along the Antimesenteric Border
- Assemble & Fire the Stapler to Create a Common Channel
- Consider Placing a Reinforcing Silk Stitch (“Crotch Stich”) at the Inner Junction – The Site of Most Tension
- Close the Enterotomies – Either with Suture or With Another Staple Load
- Close the Mesenteric Defect
- Barcelona Technique (For Ileostomy Reversal):
- Approximate Proximal & Distal Ends (Prior to Resection)
- Make Small Enterotomies at the Ends
- Pass Stapler into Both Ends to Create Common Channel
- Use Another Stapler to Amputate the Specimen
- *Benefits: Cost-Effective & Only Uses Two Staple Loads (Traditional Uses 4 Staple Loads)
- Traditional Method:
Comparison
- No Significant Difference in Outcomes Between Techniques
- No Difference Between Single-Layer vs Double-Layer Hand-Sewn Anastomoses
- No Difference Between Hand-Sewn & Stapled Anastomoses
- Possibly Higher Incidence of Radiographic Leaks When Hand-Sewn (12.2% vs 4.1%) But Not Clinical Leaks (3.2% vs 4.7%)
- Conflicting Data on Ileocolic Anastomoses (Specifically)
Intraoperative Assessment of Anastomosis Viability
- Colorectal Anastomosis Can be Endoscopically Evaluated by an Air-Leak Test
- Assessment of Perfusion;
- Historical Subjective Findings:
- Bowel Color
- Observed Pulsatile Flow at the Cut Section
- Modern Objective Findings:
- Indocyanine Green Fluorescence Angiography (ICG-FA/ICGA) – Best Studied
- Doppler US – Minimal Data
- Light Spectroscopy – Minimal Data
- Historical Subjective Findings:
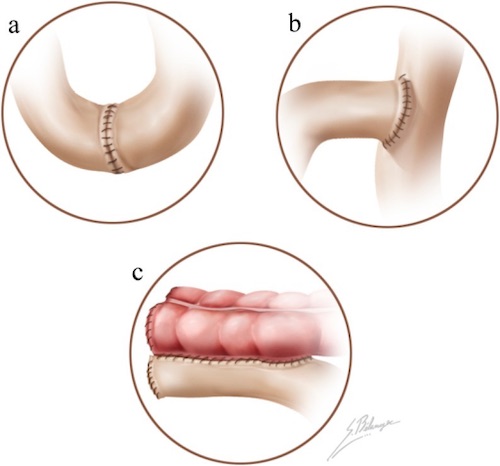
Anastomosis; (a) End-to-End, (b) End-to-Side, (c) Side-to-Side 1
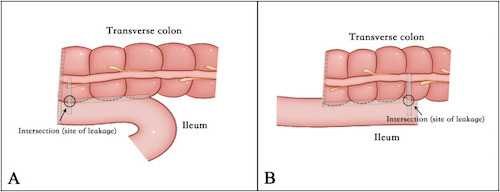
Side-to-Side Anastomosis; (A) Antiperistaltic, (B) Antiperistaltic 2
Indocyanine Green Fluorescence Angiography (ICG-FA/ICGA)
- Indocyanine Green (ICG) is a Fluorescent Probe in Response to Near-Infrared (NIR) Light
- Binds Primarily to Serum Albumin & Other Plasma Proteins
- Primarily Confined to the Intravascular Compartment with Minimal Leakage
- Excreted Almost Exclusively into Bile
- Negligible Toxicity
- Timing:
- Bowel Should Enhance < 60 Seconds
- Half-Life: 3-5 Minutes
- Cleared by Liver: 15-20 Minutes
- Dosing: Poorly Standardized
- 2-0.5 mg/kg
- 5-12.5 mg
- Imaging Systems:
- Firefly (Intuitive Surgical)
- SPY Elite (Stryker)
- PINPOINT (Stryker)
- IMAGE1 S (Karl Storz)
- D-LIGHT P SCB (Karl Storz)
- Effects on Colorectal Anastomoses: Possibly Decreased Risk of Anastomotic Leak, Reoperation & Overall Complications (Debated)
- Insufficient Data Evaluating Small Bowel Anastomoses
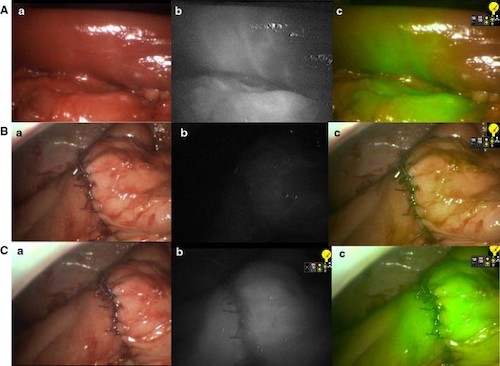
Right Hemicolectomy by ICG-FA; (A) Bowel After Vessel Division with Demarcation, (B) Anastomosis Before ICG, (C) Anastomosis After ICG; (a) Normal Light, (b) NIR, (c) Superimposition of NIR in Green 3
Anastomotic Leak
Leak Rates
- Overall: 2-7%
- Ileocolic: 1-3% (Lowest)
- Colocolic: 6-12%
- Coloanal: 10-20% (Highest)
Risk Factors
- Patient Factors:
- Male Gender
- Malnutrition
- High ASA Score
- Emergency Surgery (Compared to Elective)
- Operative Factors:
- Ischemia/Tension
- Tumor Size > 5 cm
- Multiple Stapler Firings
- Low Anastomosis (< 5 cm from Anal Verge)
- Lateral LN Dissection
- Prolonger OR (> 4 Hours)
- Debated Risk Factors:
- NSAIDs/Ketorolac (Toradol)
- Corticosteroids
- Drains
Presentation
- Abdominal Pain
- Fever
- Tachycardia
- Purulent or Feculent Drainage
- May present with an Abscess/Fluid Collection
Treatment
- Subclinical/Radiographic: Conservative Management
- Small (< 3 cm) Contained Abscess: Conservative Management & ABX
- Large (> 3 cm) or Multiloculated Abscess: Percutaneous Drain
- If Fails: Surgical Drainage
- Unstable, Peritonitis or Free Intraperitoneal Leak: Surgical Repair
References
- Terrone DG, Lepanto L, Billiard JS, Olivié D, Murphy-Lavallée J, Vandenbroucke F, Tang A. A primer to common major gastrointestinal post-surgical anatomy on CT-a pictorial review. Insights Imaging. 2011 Dec;2(6):631-638. (License: CC BY-2.0)
- Zhang M, Lu Z, Hu X, Zhou H, Zheng Z, Liu Z, Wang X. Comparison of the short-term outcomes between intracorporeal isoperistaltic and antiperistaltic totally stapled side-to-side anastomosis for right colectomy: A retrospective study on 214 consecutive patients. Surg Open Sci. 2022 Mar 26;9:7-12. (License: CC BY-NC-ND-4.0)
- Ris F, Hompes R, Cunningham C, Lindsey I, Guy R, Jones O, George B, Cahill RA, Mortensen NJ. Near-infrared (NIR) perfusion angiography in minimally invasive colorectal surgery. Surg Endosc. 2014 Jul;28(7):2221-6. (License: CC BY-4.0)