Breast: Carcinoma In-Situ
Lobular Carcinoma In-Situ (LCIS)
Basics
- Definition: Proliferation of Lobule Cells without Basement Membrane Invasion
- The Lesion Itself Is Not Premalignant (3-5% Risk of Upgrade) Mn
- Not Technically Cancer
- Creates a Bilateral Risk for Future Breast Cancer
- Overall Risk for Future Invasive Cancer: 40%
- Only 30% of Future Invasive Cancers are Invasive Lobular Carcinoma (ILC)
- 70% of Future Invasive Cancers are Invasive Ductal Carcinoma (IDC)
- Only Accounts for 15% of All Breast Cancers
Presentation
- Most Are Asymptomatic (No Lump or Pain) at Time of Diagnosis
- Most Often Found Incidentally
- Most Common in Premenopausal Women
Histologic Classification
- Classic LCIS: Proliferation of Small Cells with Cytologic Dyshesion & Intracytoplasmic Vacuoles
- Pleomorphic LCIS: Proliferation of Larger Cells with Marked Nuclear Pleomorphism
- May Demonstrate Central Necrosis & Calcifications
- Florid LCIS: Marked Distention of Involved Ducts & Lobules
- May Demonstrate Central Necrosis & Calcifications
Diagnosis
- Mammogram: Generally Does Not Cause Calcifications
- Diagnosis: Core Needle Biopsy (CNB)
- Cells are Negative for E-Cadherin (Compared to DCIS)
- Also Seen in ALH & ILC
- *See Breast: Breast Mass Evaluation
Treatment
- Primary Treatment: Surgical Excision
- Margins: No Margin Required
- May Consider Negative Margins for Pleomorphic LCIS Mn
- Behaves Similar to DCIS
- May Consider Negative Margins for Pleomorphic LCIS Mn
- Does Not Require SLNB or XRT
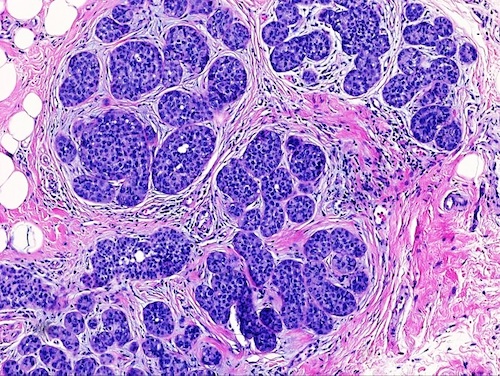
LCIS 1
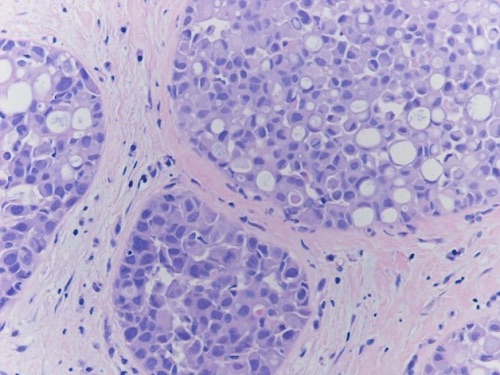
Pleomorphic LCIS 2
Ductal Carcinoma In-Situ (DCIS)
Basics
- Definition: Proliferation of Ductal Cells without Basement Membrane Invasion
- The Lesion Itself Is Premalignant
- 50% Will Become Invasive
- Poses an Ipsilateral Risk for Future Breast Cancer
Presentation
- Most Are Asymptomatic (No Lump or Pain) at Time of Diagnosis
- Most Often Found Incidentally
Diagnosis
- Mammogram: Causes Calcifications
- Diagnosis: Core Needle Biopsy (CNB)
- Cells are Positive for E-Cadherin (Compared to LCIS)
- *See Breast: Breast Mass Evaluation
Histologic Classification
- Comedo Type: Prominent Central Necrosis (Most Aggressive Type)
- Rapid Growth Past Blood Supply
- Cribriform Type: Formation of Back-to-Back Glands without Intervening Stroma
- Micropapillary Type: Intraluminal Projections Perpendicular to the Basement Membrane without Fibrovascular Cares
- Papillary Type: Intraluminal Projections Perpendicular to the Basement Membrane with Fibrovascular Cares
- Solid Type: Tumor Cells that Distend & Fill Involved Spaces without Necrosis, Fenestrations or Papillations
- *Can Also Be Classified Based on Histologic Grade (Low, Intermediate or High)
TNM Staging
- DCIS is Designated Tis (Stage 0)
Treatment
- Primary Treatment: Surgical Lumpectomy & Adjuvant Radiation Therapy
- Margins: 2 mm
- Reasoning: Spreads Along Basement Membrane So Need Margin
- If Both DCIS & Invasive Cancer are Present, Goal is “No Ink on Tumor”
- Behaves More Like Invasive Cancer
- 10-50% Require Reoperation for Close/Positive Margin
- Margins: 2 mm
- Consider Mastectomy for Patient Preference or if Adequate Margins Cannot Be Achieved by Lumpectomy
- Adjuvant Radiation Reduces Risk of Ipsilateral Recurrence by 50%
- No Survival Benefit
- Low-Risk Lesions May Consider Excision Alone without Radiation Therapy
- Does Not Require SLNB
- SLNB is Indicated if Preforming a Mastectomy (Unable to do SLNB in the Future)
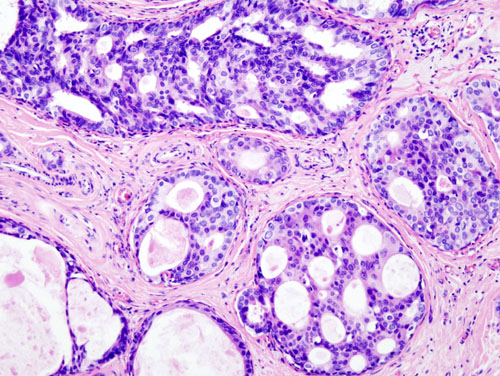
DCIS 3
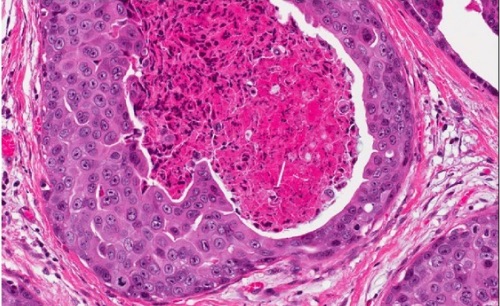
DCIS, Comedo Type 4
Mnemonics
LCIS vs DCIS
- Regarding the Lesion Itself
- L-Live: LCIS Not Premalignant
- D-Die: DCIS Premalignant
Pleomorphic LCIS Margins
- pLEO – L.E.O. (Law Enforcement Officer) is More Strict & Requires Negative Margin
References
- Ryan R, Tawfik O, Jensen R, Anant S. Wikimedia Commons. (License: CC BY-4.0)
- Wazir U, Wazir A, Wells C, Mokbel K. Pleomorphic lobular carcinomain situ: Current evidence and a systemic review. Oncol Lett. 2016 Dec;12(6):4863-4868. (License: CC BY-NC-ND-4.0)
- KGH. Wikimedia Commons. (License: CC BY-SA-3.0)
- Bane A. Ductal carcinoma in situ: what the pathologist needs to know and why. Int J Breast Cancer. 2013;2013:914053. (License: CC BY-3.0)