Breast: Breast Reconstruction
General Breast Reconstruction
Methods
- Prosthetic (Implant-Based) Reconstruction
- More Common than Autologous Reconstruction
- Less Invasive
- Faster Surgery
- Faster Recovery
- Autologous (Flap-Based) Reconstruction
- Uses Own Tissue
- More Invasive with Longer Recovery
- Requires Sufficient Excess Tissue for Reconstruction
- Source: Generally from the Abdomen, Although Occasionally Can Come from the Thigh or Back
Reconstruction Timing
- Immediate Reconstruction
- Generally Preferred
- Contraindication: Future Radiation Therapy
- Delayed Reconstruction
- More Difficult Once Tissues Have Healed
- May Have Worse Cosmetic Outcome
Choice of Reconstruction Method
- History of Radiation Therapy to the Chest:
- Autologous Reconstruction is Generally Preferred
- Permanent Vascular Injury Increases Complication Rates for Prosthetic Reconstructions
- Risk of Expander Failure: 30-40%
- Planned Adjuvant Radiation Therapy to the Chest:
- Options:
- Delayed Reconstruction Alone (Will Leave Flat Chested for a Period of Time)
- Temporary Expander with Delayed Removal & Reconstruction
- Immediate Autologous Flap with Have Irreversible Changes from Radiation & Should Be Avoided
- Options:
- No Radiation:
- Choice Based on Patient Preference
General Complications
- Pain
- Hematoma/Seroma
- Infection
- Skin Necrosis
- 18-30% Risk Following Immediate Reconstruction
- Prevention:
- Preserve Subdermal Plexus
- Gentle Retraction of Skin Flaps
- Minimize Thermal Damage
- Treatment: Excision of Necrotic Tissue Once Completely Demarcated

Breast Implant 1
Prosthetic (Implant-Based) Reconstruction
Location/Approach
- Sub-Pectoral Approach
- Prosthesis is Placed Under the Pectoralis Muscle
- Immediately Limited Volume Possible Due to Tightness of the Muscle
- Tissue Expanders Allow Increased Possible Volume Over Time
- Originally the Approach was Cosmetically Higher than a Normal Breast
- Now an Acellular Dermal Matrix Can Be Used to Place in a More Normal Location (Requires Cutting of the Pectoralis Muscle Which Can Cause Animation Deformity)
- Pre-Pectoral Approach
- Historically was Abandoned Due to Risk for Increased Flap Necrosis/Infection
- Now Increasing in Popularity Due to Better Skin Flaps Than in the Past
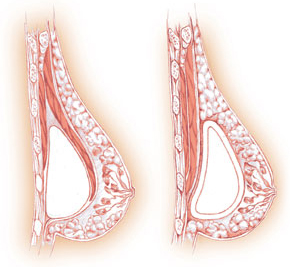
Sub-Pectoral (Left), Pre-Pectoral (Right) 2
Tissue Expanders
- Initially Placed to Fill the Cavity Prior to Placing the Actual Prothesis
- Intermittently Filled Over the Course of a Few Months
- Benefits:
- Allows Monitoring of Skin Flaps to Ensure Viability Prior to Placing the Definitive Prosthesis
- Allows Increased Available Volume for Definitive Prosthesis Placement Under the Pectoralis Muscle
- May Consider Immediate Placement of Prosthesis without Expander if Confident in Flap Vasculature
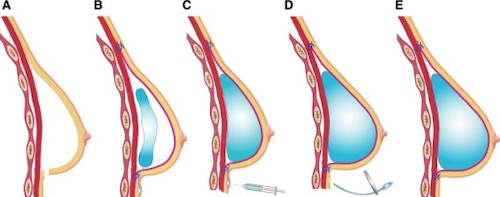
Tissue Expander Sequentially Filled 3
Prosthetic Types
- Material:
- Saline
- Silicone Shell Filled with Saline
- Rupture is Generally Safer
- Silicone
- Feels More Natural (Most Commonly Chosen by Patients)
- Possibly Concerned for Increased Risk of Autoimmune Diseases (Still Debated)
- Saline
- Shape:
- Round
- Smooth Surface without Texture
- Shaped (Tear-Drop Shape)
- Requires a Textured Coating to Prevent Migration & Polarity Changes
- Texture Can Induce a Lymphoproliferative Disorder Which Can Progress to Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL)
- Generally Avoided Now Due to Concern for Texture
- Round
Specific Complications
- Capsular Contracture
- Prothesis Develops a Fibrous Capsule
- Can Present Months-Years After Placement
- Baker Classification:
- Class I: Breast Soft with No Palpable Capsule & Looks Normal
- Class II: Breast A Little Firm with Palpable Capsule but Looks Normal
- Class III: Breast Firm with Easily Palpable Capsule & Visually Abnormal
- Class IV: Breast Hard, Cold, Painful & Markedly Distorted
- Treatment:
- Initial Management: Massage
- May Consider Medications (Zafirlukast, Vitamin E & Topical Diclofenac)
- Open Capsulotomy May Be Required for Class III-IV Disease
- Total Capsulotomy Preferred Over Anterior-Only (Lower Rate of Recurrence)
- Initial Management: Massage
- Rupture
- Presentation:
- Saline – Will Reabsorb & Demonstrate Flattening
- Silicone – Will Stay Localized Causing More Difficulty in Identifying the Rupture
- Can Migrate Through the Lymph Nodes
- Monitoring for Silent Rupture: MRI 3 Years After Surgery & Then Every 2 Years for Life
- Treatment: Excision of Implant
- Presentation:
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL)
- Increased Risk with Increased Degree of Prosthetic Texture
- Can Still Develop Even After Prosthetic Removal
- Presentation: A Persistent Delayed Seroma Appearing Years After the Implant Placement
- Diagnosis: Needle Aspiration of Seroma Fluid
- Cytology Showing Anaplastic Large Cells & CD-30 T Cells on Flowcytometry
- Treatment: Surgical Excision (80-90% Success)
- Increased Risk with Increased Degree of Prosthetic Texture
- Breast Implant Illness (BII)
- Constellation of Nonspecific Symptoms:
- Autoimmune Disorders (Rheumatoid Arthritis, Sjogren’s Syndrome, etc.)
- Fatigue
- Fibromyalgia
- May Be Associated with Silicone-Based Implants (Debated)
- Constellation of Nonspecific Symptoms:

Capsular Contracture 4
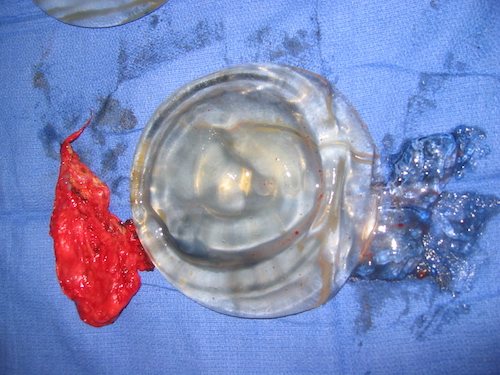
Ruptured Implant 5
Autologous (Flap-Based) Reconstruction
Basics
- Abdominal Wall Flaps are Generally Preferred
- Transfer:
- Free Flap: Supplying Vasculature is Transected & Re-Implanted
- Pedicle Flap: Tissue Moved with Vascular Pedicle Preserved
Abdominal Wall Flaps
- Transverse Rectus Abdominis Myocutaneous (TRAM) Flap
- Transfers Skin, Subcutaneous Tissue & Rectus Abdominis Muscles
- Relies on Superior Epigastric Vessels
- Higher Risk for Abdominal Wall Diastasis or Hernia Due to Loss of Muscle
- Best Determinant of Flap Viability: Periumbilical Muscle Perforators
- Deep Inferior Epigastric Perforator (DIEP)/Fasciocutaneous Flap
- Transfers Only Skin & Subcutaneous Tissue (Spares Muscle)
- Better for Donor Site; Fascia Stays Intact
- Less Pain/Nerve Damage & Lower Hernia Chance
- Microsurgery – Much Longer
- Can Provide Good Symmetry if Native Contralateral Breast
- Superficial Inferior Epigastric Artery (SIEA) Flap
- Transfers Only Skin & Subcutaneous Tissue
- Spares the Deep Epigastric Artery – Thereby Avoids Any Muscle Incisions (Compared to DIEP)
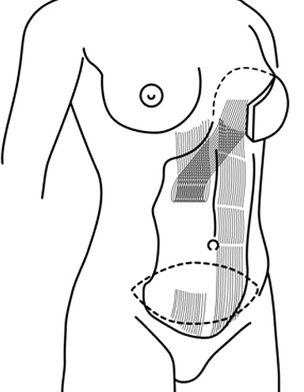
TRAM Flap 6
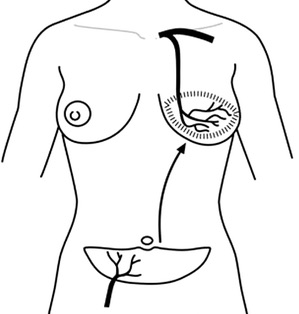
DIEP Flap 6
Posterolateral Flaps
- Latissimus Dorsi Myocutaneous Flap (LDMF)
- Transfers Skin, Fat & A Portion of the Latissimus Dorsi Muscle
- Provides a Smaller Total Volume & Almost Always Requires Additional Implant for Adequate Cosmesis
- Thoracodorsal Artery Perforator Flap (TDAP)
- Transfers Only Skin & Fat from the Back
Other Autologous Options
- Superior Gluteal Artery Perforator (SGAP) Flap
- Transfers Skin & Fat from the Superior Buttock
- Muscle-Sparing
- Inferior Gluteal Artery Perforator (IGAP) Flap
- Transfers Skin & Fat from the Inferior Buttock
- Muscle-Sparing
- Less Common than SGAP
- Profunda Artery Perforator (PAP) Flap
- Transfers Skin & Fat from the Upper Posterior Thigh
- Muscle-Sparing
- Transverse Upper Gracilis (TUG) Flap
- Transfers Skin, Fat & Gracilis Muscle from Inner Upper Leg
- Fat Grafting (Autologous Fat Transfer)
- Adipose Tissue Removed from Distant Source by Liposuction, Processed into a Liquid & Transferred to the Breast
- Removed from Abdomen, Thigh & Buttock
- Transferred Fat is Often Reabsorbed with Loss of Volume Over Time (Often Lose About 50% of Volume)
- Adipose Tissue Removed from Distant Source by Liposuction, Processed into a Liquid & Transferred to the Breast
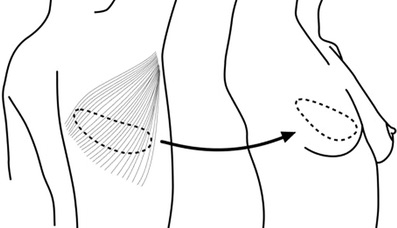
LDMF Flap 6
References
- FDA. Wikimedia Commons. (License: Public Domain)
- Dr Roudner. Wikimedia Commons. (License: CC BY-SA-4.0)
- Becker H, Lind JG 2nd, Hopkins EG. Immediate Implant-based Prepectoral Breast Reconstruction Using a Vertical Incision. Plast Reconstr Surg Glob Open. 2015 Jul 8;3(6):e412.(License: CC BY-NC-ND-3.0)
- Khoo LS, Radwanski HN, Senna-Fernandes V, Antônio NN, Fellet LL, Pitanguy I. Does the Use of Intraoperative Breast Sizers Increase Complication Rates in Primary Breast Augmentation? A Retrospective Analysis of 416 Consecutive Cases in a Single Institution. Plast Surg Int. 2016;2016:6584810.(License: CC BY-4.0)
- Dr Oliver. Wikimedia Commons. (License: Public Domain)
- Dialani V, Lai KC, Slanetz PJ. MR imaging of the reconstructed breast: What the radiologist needs to know. Insights Imaging. 2012 Jun;3(3):201-13. (License: CC BY-2.0)