Trauma: Cardiac Trauma
Cardiac/Pericardial Injury
AAST Heart Injury Scale
- *See AAST
- Injury Scale is Under Copyright
Myocardial Contusion/Blunt Cardiac Injury (BCI)
- Most Common Complication: Arrhythmia
- Most Common Arrhythmia: SVT
- Most Common Cause of Death: VT/VF
- Not Predicted by Sternal Fracture
- Screening:
- Initial Screen: ECG
- Most Common Dysrhythmia: PVC’s
- If ECG Abnormal: Echocardiogram & Telemetry for 24-48 Hours
- May Forego Formal Echo if FAST is Able to Rule Out Pericardial Effusion or Other Causes of Shock
- If Hemodynamically Unstable or Arrhythmia Persistent: Echocardiogram
- Transesophageal Echo (TEE) May Be Preferred Over Transthoracic Echo (TTE) if Available
- If Echo Abnormal: Send to ICU
- CK-MB, CPK & Nuclear Imaging are Not Useful
- Initial Screen: ECG
Cardiac Laceration/Perforation
- Most Common Injury:
- Penetrating Trauma: Right Ventricle
- Due to Anterior Position
- Blunt Trauma: Right Atrium #1, Right Ventricle #2
- Penetrating Trauma: Right Ventricle
- Muscular Ventricle May Seal Lacerations Preventing Exsanguination Prior to Arrival
- Tx: Median Sternotomy & Cardiorrhaphy (Primary Repair)
- Use Non-Absorbable Monofilament Suture with Pledgets, Typically a Horizontal Mattress
- With Anterior Injury, Posterior Heart Must Also Be Inspected
Coronary Artery Injury
- Most Common Vessel Injured: Left Anterior Descending (LAD)
- Tx:
- Proximal/Middle: Cardiopulmonary Bypass & CABG
- Use Saphenous Vein
- *Consider Primary Repair if There is No Loss of Length
- Distal: Ligation
- Proximal/Middle: Cardiopulmonary Bypass & CABG
Blunt Traumatic Pericardial Rupture (BTPR)
- Can Cause Cardiac Herniation or Hemothorax
- Heart Can Herniate into Pleural Cavity or Abdomen
- Rupture Often Relieves Potential Tamponade
- High Mortality Due to Associated Injuries & Often Discovered at Autopsy
- Overall Survival Rate: 24%
- Survival Rate if Isolated: 67%
- Presentations:
- Herniation Mimics Pericardial Tamponade Due to Decreased Venous Return
- Consider if Unstable with HTX & Negative FAST but High Concern for Cardiac Injury
- May See Sudden Loss of When Patient is Moved or Placed on a Stretcher Due to Herniation
- May See an “Empty” Pericardial Cavity on Left Thoracotomy if Herniated into Right Pleural Cavity
- Herniation Mimics Pericardial Tamponade Due to Decreased Venous Return
- Tx: Median Sternotomy
- May Also Be Repaired by Laparotomy or Thoracotomy if Done for Other Reasons
- Replace Heart into Pericardial Cavity if Displaced
- Management of Pericardial Tear:
- Primary Repair (Interrupted Nonabsorbable Suture) – Generally preferred
- Can Use a Prosthetic Patch if Too Large to Close Primarily
- Small Defects Can Be Left Alone if Herniation is Not Possible
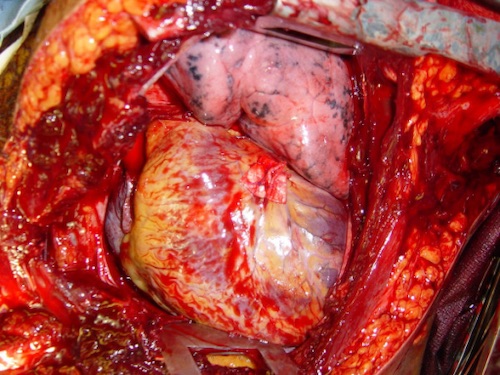
Cardiorrhaphy with Pledgets 1
Cardiac Tamponade
Basics
- Cardiac Filling Impeded by Pericardial Fluid
- Can Occur with Only A Small Amount of Blood
- Serves a Protective Effect in Penetrating Cardiac Injury
- Limits Extra-Pericardial Hemorrhage
- Non-Traumatic: *See Cardiothoracic Surgery: Pericardial Effusion & Cardiac Tamponade
Phases
- I: Increased Pericardial Pressure
- Output Maintained by Tachycardia, Increased SVR & Filling Pressure
- II: Diminished Cardiac Output
- III: Intrapericardial Pressure Approaches Ventricular Filling Pressure
- See Cardiac Arrest from Profound Coronary Hypoperfusion
Presentation
- Sx: Chest Pain & Dyspnea
- Pulsus Paradoxus: Decreased BP > 10 During Inspiration (Normal < 10)
- Beck’s Triad:
- JVD
- Muffled Heart Sounds
- Hypotension with Narrow Pulse Pressure
- Kussmaul’s Sign: JVD Upon Inspiration
- First Sign: Decreased Right Atrium Filling
Diagnosis
- Dx: Clinical vs Echo/FAST
- Subxiphoid Pericardial Window
- Diagnostic, Not Therapeutic
- Rarely Preformed Now; But Consider if FAST Equivocal
- Procedure:
- 10 cm Midline Incision Over Xiphoid
- Dissect toward Cardiac Impulses to Find Pericardium
- Grasp Pericardium Between Two Alice Clamps
- 1-2 cm Longitudinal Incision in Pericardium
- Field Flooded with Fluid
- Results:
- Positive: Bloody Fluid
- Clotted Blood May Be Dry on Incision
- Negative: Clear/Straw-Colored Fluid
- Positive: Bloody Fluid
Treatment
- Primary Tx: Median Sternotomy
- Avoid Intubation Until in the OR & Already Prepped – May Crash After Anesthetic Induction
- Pericardiocentesis: To Temporize for Transfer or If Acutely Unstable Prior to OR
- Used More Often in Non-Traumatic Causes
- Insertion: 18-Gauge Spinal Needle
- Subxiphoid; Under Xiphoid & Toward Left Shoulder
- Parasternal; Left 5th/6th Rib Space & Perpendicular
- Apical; Left 5th/6th Rib Space, 5 cm Lateral & Toward Right Shoulder
- *In General, In Trauma, Blood in the Pericardium Does Not Clot – Clotted Blood Would Indicate Aspiration of a Cardiac Chamber
- ED Thoracotomy: For Traumatic & Sudden Decompensation
- Non-Traumatic Tx: *See Cardiothoracic Surgery: Pericardial Effusion & Cardiac Tamponade
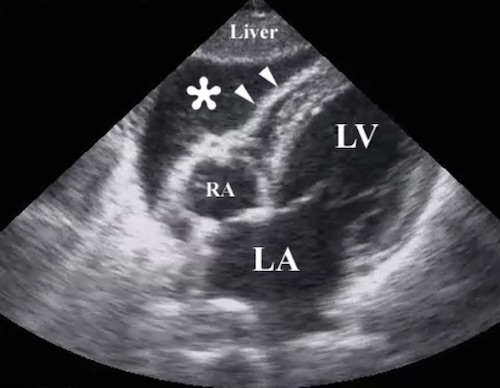
Cardiac Tamponade on FAST 2
References
- Cothren CC, Moore EE. Emergency department thoracotomy for the critically injured patient: Objectives, indications, and outcomes. World J Emerg Surg. 2006 Mar 24;1:4. (License: CC BY-2.0)
- Gillman LM, Ball CG, Panebianco N, Al-Kadi A, Kirkpatrick AW. Clinician performed resuscitative ultrasonography for the initial evaluation and resuscitation of trauma. Scand J Trauma Resusc Emerg Med. 2009 Aug 6;17:34. (License: CC BY-2.0)