Vascular: Carotid Endarterectomy (CEA)
Carotid Endarterectomy (CEA)
Basics
- Open Surgery to Remove Carotid Plaque
- Goal: Prevent Future Stroke
Positioning
- Neck Extended & Rotated to Contralateral Side
- Arms at Side
Procedure
- Initial Incision
- Standard: Longitudinal Along Medial Sternocleidomastoid Muscle (SCM)
- Transverse: 1-2 cm Below Angle of Jaw
- Technically May Be More Difficult
- Primarily for Cosmesis
- Expose Carotid Sheath
- Divide Platysma
- Mobilize Medial Border of SCM
- Avoid Injury to External Jugular Vein
- Avoid Injury to Greater Auricular Nerve
- Enter Carotid Sheath
- Minimize Carotid Artery Manipulation (Embolization Risk)
- Dissect Medial Border of Internal Jugular Vein (IJV)
- Divide Facial Vein (Seen Crossing Medially)
- Retract IJV Laterally
- Identify Vagus Nerve (Between IJV & Carotid; May Lie Anteriorly)
- Dissect Carotid Artery
- Identify Common Carotid Artery (CCA), External Carotid Artery (ECA) & Internal Carotid Artery (ICA)
- Dissect ICA Past Area of Stenosis
- Avoid Injury to Carotid Body at Bifurcation
- Identify Structures
- Ansa Cervicalis (Medial to CCA)
- Superior Thyroid Artery (Off Proximal ECA)
- Hypoglossal Nerve (Superior Extent)
- Control Inflow & Outflow Circumferentially
- CCA with Umbilical Tape & Rummel’s Tourniquet
- Superior Thyroid Artery with Vessel Loops
- Or Tie
- ECA & ICA with Vessel Loops
- Identify Common Carotid Artery (CCA), External Carotid Artery (ECA) & Internal Carotid Artery (ICA)
- Clamping Mn
- First Administer 70-100 U/kg Heparin
- Allow 3 Minutes Circulation
- First Clamp ICA (Prevent Embolization)
- Ensure on Normal Portion of Artery Distal to Plaque
- Then Clamp CCA
- Then Clamp ECA Last
- First Administer 70-100 U/kg Heparin
- Preform Endarterectomy
- Close
- Close Platysma
- Close Skin
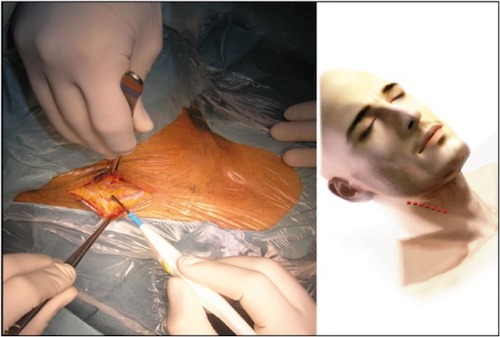
CEA Incision 1

Clamping (I.C.E.) 1
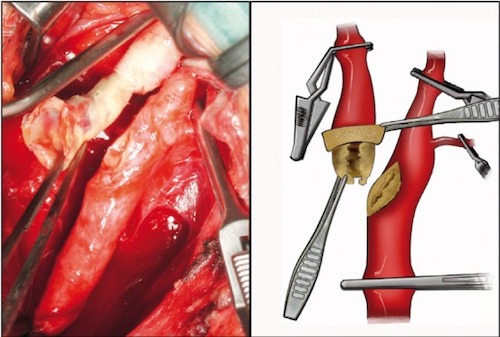
Conventional Endarterectomy
- Vertical Arteriotomy
- From CCA into ICA
- If Shunt Used:
- First Place into Distal ICA & Back Bled
- Then Proximal End Placed into CCA
- Endarterectomy
- Begin in CCA (Between Media & Adventitia)
- Remove Intima and Part of Media
- Continue into ICA
- #1 Concern: Ensure a Good Distal End Point
- Endpoint at Normal Intima with Gradual Tapering
- Extend into ECA Orifice with Gradual Tapering
- Begin in CCA (Between Media & Adventitia)
- Close with Patch (Autologous, PTFE, Dacron or Bovine)
- Prior to Closure: Vessels Bled & Site Irrigated with Heparinized Saline
- *In General Patch Represents Standard of Care Although Some Now Suggest Selective Patching if Diameter ≥ 6 mm (Debated)
- Release Clamps
- First Release ICA Clamp Briefly to Back Bleed
- Then Replace
- Then Release Clamps on ECA and CCA (Remaining Air/Debris to ECA)
- Finally Remove ICA Clamp
- First Release ICA Clamp Briefly to Back Bleed
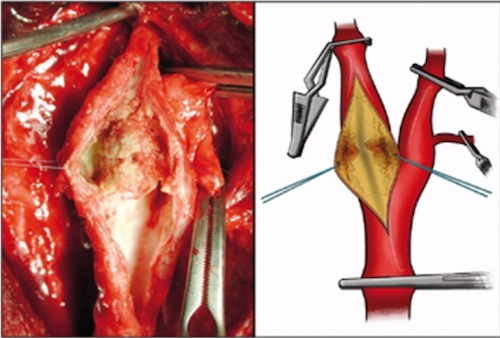
Conventional Endarterectomy 1
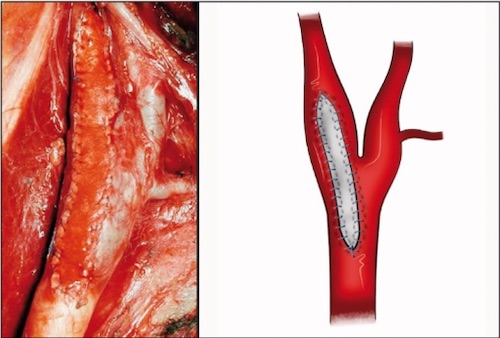
Patch Angioplasty 1
Eversion Endarterectomy
- Completely Transect the ICA at the Bifurcation
- Adventitia is Then Everted Circumferentially (“Circumcised”) Back Off the Carotid Plaque
- Plaque Then Removed from the Common Carotid
- ICA Re-Anastomosed to the Bifurcation by Simple End-to-End Anastomosis
- No Patch Required
- *Similar Results/Complications Between Conventional & Eversion Techniques
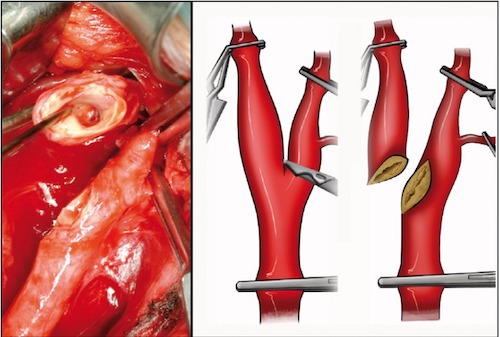
Eversion Arterial Transection 1
Eversion Endarterectomy 1
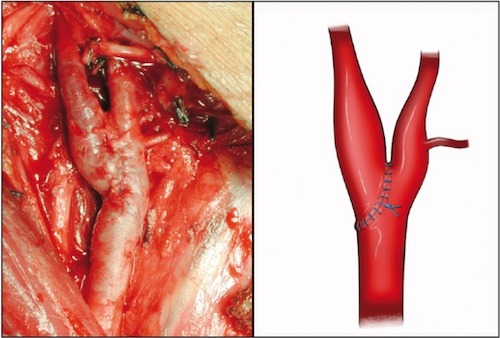
Eversion Closure 1
Bilateral Repairs
- First Repair: Side with Greatest Stenosis
- If Equal: Dominant Side First
- Before Advancing to Second Contralateral Side: Verify Intact Ipsilateral Side
Carotid Endarterectomy (CEA) – Complications
Perioperative Stroke
- Often from Residual Flap or Thrombosis
- Mostly Reversible to Flow Restored within 1-2 Hours
- Management:
- Intraoperative (Waking in OR): Reexplore
- Postoperative: Will Likely Require Reexploration in OR
- Consider Duplex US if Rapidly Available
- If US Negative: CT Head (Rule Out Hemorrhage)
Restenosis
- Risk: 5-20%
- Causes:
- Immediate (< 4 Weeks): Technical Error
- Early (1 Month-2 Years): Myointimal Hyperplasia
- Late (> 2 Years): Recurrent Atherosclerosis
- Treatment:
- Asymptomatic: Conservative Management
- Symptomatic: Stent vs Repeat CEA
Myocardial Infarction (MI)
- Most Common Non-CVA Morbidity
- Causes 25-50% of Perioperative Deaths
Cranial Nerve Injury (CNI)
- Most Are Transient & Resolve After a 3-4 Weeks
- Risk of Injury: 5-20%
- Risk of Permanent Injury: 0-1%
- Most Common Injury: Vagus (#1) & Hypoglossal (#2)
- Most Injuries are Transient
- Specific Nerve Injuries:
- Hypoglossal Nerve
- Lies Just Above the Bifurcation
- Presentation: Speech & Mastication Deficit
- Tongue Deviates to Ipsilateral Side of Injury
- RLN/Vagus
- The Most Dangerous Nerve Injury
- Lies Within the Carotid Sheath
- Presentation: Hoarseness
- Typically from Vascular Clamping
- Glossopharyngeal
- Rare; Most Common with High Dissections
- Presentation: Swallowing Difficulty
- Ansa Cervicalis
- Presentation: Strap Muscle Deficits
- Facial Nerve (Marginal Mandibular Branch)
- Presentation: Smiling Deficit
- From Corner of Mouth Retraction
- Typically from Excessive Superior Retraction
- Presentation: Smiling Deficit
- Greater Auricular Nerve
- Presentation: Numb Earlobe
- Hypoglossal Nerve
Cerebral Hyperperfusion Syndrome
- Impaired Autoregulation of Cerebral Perfusion After Chronic Hypoperfusion
- Risk: 0.3-1.0%
- High Mortality (75-100%)
- Risk Factors:
- Preoperative High-Grade Stenosis
- Postoperative Hypertension
- Bilateral Staged
- Presentation:
- Hypertension
- Ipsilateral Frontal Headache
- Stroke & Seizure
- Tx: Antihypertensives & Anti-Seizure Meds
Postoperative Hematoma
- Risk: 1-3%
- Mostly from Diffuse Oozing
- Creates a Risk Tracheal Compression & Airway Loss
- Treatment: Emergent Intubation & Open in OR
- *Open at Bedside (As in Thyroidectomy) Only in an Absolute Emergency – Possibility of Graft Blowout that Needs Repair in OR
Pseudoaneurysm
- Presents as a Pulsatile Mass
- Treatment: Surgical Repair
- Drape/Prep Before Intubation
Carotid Body Injury
- Presentation: HTN
- Treatment: Nitroprusside (Avoid Bleeding)
Mnemonics
Clamping Order for CEA
- “ICE”
- ICA (First)
- CCA (Second)
- ECA (Last)
- Unclamp in the Opposite Order
References
- Chiesa R, Melissano G, Castellano R, Tshomba Y, Marone EM, Civilini E, Astore D, Calliari F, Catenaccio B, Coppi G, Carozzo A, Mennella R. Carotid Endarterectomy: experience in 8743 cases. HSR Proc Intensive Care Cardiovasc Anesth. 2009;1(3):33-45. (License: CC BY-NC-3.0)