Biliary Tract: Cholecystitis
Cholecystitis
Basics
- Cystic Duct Obstruction
- Initially Sterile Inflammation Until Secondarily Infected
- Most Common Organism: E. coli
Presentation
- RUQ Pain
- Murphy’s Sign – Sudden “Catch” During Inspiration with Gentle RUQ Pressure
- Boas Sign – Hyperesthesia (Increased Sensitivity) Below the Right Scapula on Back
- Nausea & Vomiting
- Fever
- Leukocytosis
Diagnosis
- Diagnosis: US 95% Sensitive
- Labs:
- Most Sensitive Lab: CCK-Hida
- LFT’s Normal or Only Slightly Elevated
- Important to Rule Out Choledocholithiasis During Work-Up
Tokyo Guidelines – Severity Classification
- Grade I (Mild): No Organ Dysfunction & Limited Disease in Gallbladder
- Cholecystectomy Low-Risk
- Grade II (Moderate): No Organ Dysfunction but Extensive Disease in Gallbladder
- Cholecystectomy May be More Difficult
- Characterized by Leukocytosis, Palpable-Tender Mass, Duration > 72 Hours & Significant Inflammation on Imaging
- Grade III (Severe): Organ Dysfunction Present
Treatment
- General Treatment: Early Cholecystectomy
- Early (< 72 Hours) vs Late (7-45 Days) Cholecystectomy:
- Early Has Shorter Length of Stay, Fewer Work Days Lost, Lower Total Costs & Less Wound Infection
- Similar Complications, Conversion to Open, CBD Injury Rate and Mortality
- No Benefit to “Cooling Off Period”
- If Unstable or Unfit for Surgery: Percutaneous Cholecystostomy Tube
- 90% Effective at Relieving Symptoms
- Repeat Cholecystogram in 3-6 Weeks
- Contrast Injected Through Catheter
- Can Remove Catheter if Cystic Duct Patent
- Strongly Consider Elective Interval Cholecystectomy
Pregnancy Considerations
- First Trimester: Medical Management (NPO/ABX)
- 85-95% Effective
- If Fails: Percutaneous Cholecystostomy Tube as Bridge to Second Trimester Cholecystectomy
- Surgery Risks Fetal Organogenesis
- Second Trimester (13-26 Weeks): Cholecystectomy
- Third Trimester: Medical Management (NPO/ABX)
- If Fails: Percutaneous Cholecystostomy Tube as Bridge to Postpartum Cholecystectomy
- Surgery Risks Preterm Labor

Cholecystitis with Thickened Wall on US 1
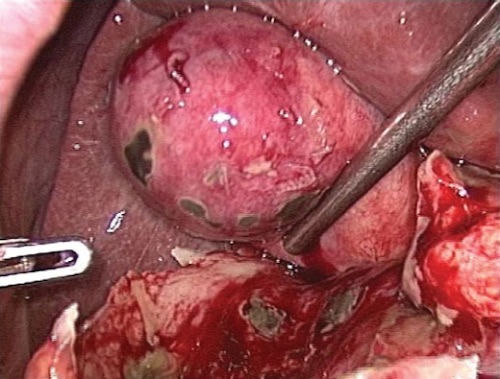
Gangrenous Gallbladder at Surgery 2
Emphysematous Cholecystitis
Basics
- Infection by Gas-Forming Organisms
- More Common in Diabetics & Elderly Men
- Often Heralds Development of Gangrene, Perforation or Other Complications
- Gallbladder Complications
- 75% are Gangrenous
- 20% are Perforated
- Mortality: 25%
Organisms
- Clostridium perfringens (GPR) – Most Common
- E. coli – Second Most Common
Treatment
- Stable: Emergent Cholecystectomy
- Unstable: Cholecystostomy Tube

CT Showing Emphysematous Cholecystitis 3
Acalculous Cholecystitis
Basics
- Gallbladder Inflammation Without Stones
- From Biliary Stasis, Increased Viscosity & Ischemia
- Often Present in Otherwise Ill Patients
Risk Factors
- Trauma
- Burns
- Surgery
- AIDS
- Infection or Sepsis
- CPR
- TPN
- Diabetes
- Immunosuppression
- Childbirth
Diagnosis
- Diagnosis: US
- If Uncertain: HIDA
- Morphine Decreases False Positive Rate
- If Critically Ill: US Sufficient, Do Not Wait for HIDA
Treatment
- Stable: Cholecystectomy
- If Unstable or Unfit for Surgery: Percutaneous Cholecystostomy Tube
- If Fails: Cholecystectomy
- Delayed Cholecystectomy Not Necessary Once Cholecystitis Resolved & Acute Illness Improves (No Stones)
References
- Cwik G, Skoczylas T, Wyroślak-Najs J, Wallner G. The value of percutaneous ultrasound in predicting conversion from laparoscopic to open cholecystectomy due to acute cholecystitis. Surg Endosc. 2013 Jul;27(7):2561-8. (License: CC BY-4.0)
- Gomes RM, Mehta NT, Varik V, Doctor NH. No 72-hour pathological boundary for safe early laparoscopic cholecystectomy in acute cholecystitis: a clinicopathological study. Ann Gastroenterol. 2013;26(4):340-345. (License: CC BY-NC-SA-3.0)
- Sunnapwar A, Raut AA, Nagar AM, Katre R. Emphysematous cholecystitis: Imaging findings in nine patients. Indian J Radiol Imaging. 2011 Apr;21(2):142-6. (License: CC BY-NC-SA-3.0)