Esophagus: Fundoplication
Fundoplication – Types
Nissen Fundoplication Procedure
- Position in Steep Reverse Trendelenburg
- Mobilize the Esophagus
- Divide the Gastrohepatic Ligament – Initial Landmark
- Watch for Replaced Left Hepatic Artery
- Bluntly Mobilize the Right Crus
- Preserve the Anterior Vagus Nerve
- Keep Peritoneal Covering Over the Crura (Stripping Will Weaken the Repair)
- Bluntly Mobilize Circumferentially Around the Esophagus Until 3-5 cm Are in the Abdomen Without Tension
- Divide the Gastrohepatic Ligament – Initial Landmark
- Divide Short Gastrics to Mobilize the Fundus
- Stay Off Stomach to Prevent Thermal Injury
- Avoid Injury to Spleen by Tearing the Capsule
- Approximate Crura
- Permanent Interrupted Sutures
- Indications for Mesh Not Well Defined (Never Use Synthetic Mesh – Risk for Erosion)
- May Require Diaphragmatic Relaxing Incision
- Wrap Gastric Fundus Posterior 360-Degrees
- Use Three Interrupted Permanent Stitches
- Create Wrap Using the Fundus, Not the Gastric Body
- Wrap Should be 2-3 cm Short & “Floppy” to Minimize Postoperative Side Effects
Partial Fundoplication
- Approach Mn
- Dor Fundoplication
- Anterior 180-Degrees
- Toupet Fundoplication
- Posterior 270-Degrees
- Dor Fundoplication
- Better if Concurrent Dysmotility
- Prevents Worsening
Belsey Mark IV Repair
- Fundoplication Preformed Through a Thoracotomy Mn
- Anterior 240-Degrees
- Potential Indications:
- Hostile Abdomen
- Short Esophagus – Able to Free More Esophagus
- Massive Hiatal Hernia
- Morbid Obesity
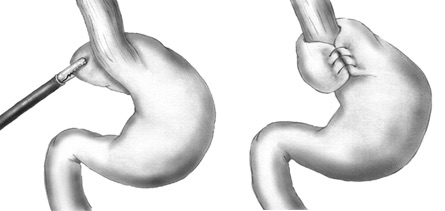
Nissen Fundoplication 1
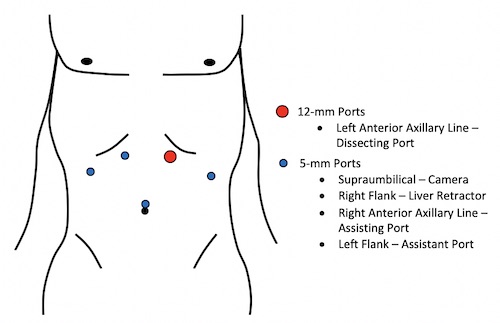
Nissen Port Placement
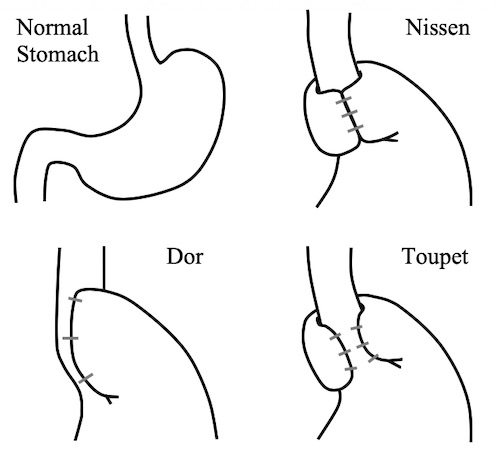
Fundoplication Types
Fundoplication – Adjuncts
Collis Gastroplasty
- Single Linear Staple Along Stomach Cardia to Create a 4-5 cm Neo-Esophagus
- First Insert a 45-48 French Bougie to Maintain Adequate Patency
- Indication: Unable to Obtain Adequate Intraabdominal Esophagus Length
- Minimum 3 cm
- Only Needed in 2-5% of Cases
- Extended Mediastinal Dissection/Mobilization is Most Often Sufficient for Lengthening
- Approaches:
- Open
- Combined Thoracoscopic-Laparoscopic
- Linear Stapler Inserted Through the Thorax After Thoracoscopy Used to Confirm No Adhesions/Obstruction
- Left Generally Preferred
- Total Laparoscopic
- Original Description: 25 mm Circular Stapler Fired 3 cm Below the Angle of His to Allow Passage of a Linear Stapler (Rarely Done Now)
- Wedge-Collis Gastroplasty (Wedge-Fundectomy): Wedge Resection of Fundus Opposed to Single Staple Line
Hill Esophagogastropexy
- Indication: Antireflux Surgery with Inadequate Fundus Length for Wrap
- Possibly Due to Prior Gastric Surgery
- Procedure:
- Plication of Lesser Curvature Around the Right Side of the Esophagus
- Esophagogastropexy to the Median Arcuate Ligament
- Requires Intraoperative Manometry
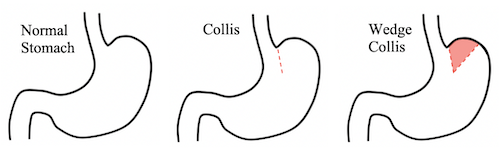
Collis Gastroplasty
Fundoplication – Complications
Dysphagia
- Most Self-Resolve in 4-12 Weeks
- Strongest Predictor of Postoperative Dysphagia: Preoperative Dysphagia
- Most Common Cause: Postoperative Edema
- Most Common Cause Requiring Surgery: Wrap Too Tight
- Tx: Liquid/Soft Diet Until Symptomatic Resolution
- If Fails: Dilation
- If Unable to Tolerate Secretions Requires Return to the OR Due to Wrap Being Too Tight
Gas Bloat Syndrome
- Wrap Causing Inability to Belch Air
- Causes Bloating and a Buildup of Gas Within the Stomach
- Cause: Wrap Too Tight
- Usually Self-Limiting Within a Few Weeks
- Tx: Lifestyle Modification
- Avoid Aerophagia, Straws & Carbonated Beverages
- Possible Medications: Simethicone, Metoclopramide or Erythromycin
- Options if Fails:
- Conversion to Partial Wrap
- Endoscopic Pneumatic Dilation
- If Diagnosed Gastroparesis: Pyloroplasty, Pyloric Botox Injection or Pneumatic Pyloric Dilation
Recurrent GERD
- Most Patients with Recurrent Symptoms Do Not Have Documented Reflux on pH Testing
- Tx: PPI vs Surgical Revision
Wrap Failure
- Persistent, Recurrent or New-Onset Symptoms
- Rate: 10-15%
- Most Occur within 2 Years
- Categories
- Transhiatal Fundoplication Herniation – Most Common Cause of Failure (47-61%)
- Fundoplication Disruption
- Slipped Fundoplication
- Tight Wrap/Crural Stenosis
- Technical Failure: Twisted Wrap or Malpositioned
- Most Common Technical Failure: Use of Gastric Body Instead of the Fundus for the Wrap
Postop EGD Findings
- Nissen Fundoplication: Circumferential Transverse Gastric Fold Involving the Cardia
- Resembles a “U”
- Creates a Stacked Coil Appearance
- Partial Fundoplication: Transverse Gastric Fold Partially Involving the Cardia
- Resembles a Greek Omega (“Ω”)
- Disrupted Fundoplication: Transverse Gastric Fold Does Not Involve the Shaft of the Endoscope
- Occasionally Unable to Even See a Transverse Gastric Fold
- Twisted Fundoplication: Gastric Fold in an Oblique Position
- Migrated Fundoplication: Fundoplication Migrated Above the Diaphragm into the Thorax
- Slipped Fundoplication: GEJ > 2 cm Above the Zone of Pressure
- Paraesophageal Hernia: Intact Fundoplication with Enlarged Hiatus with Herniation
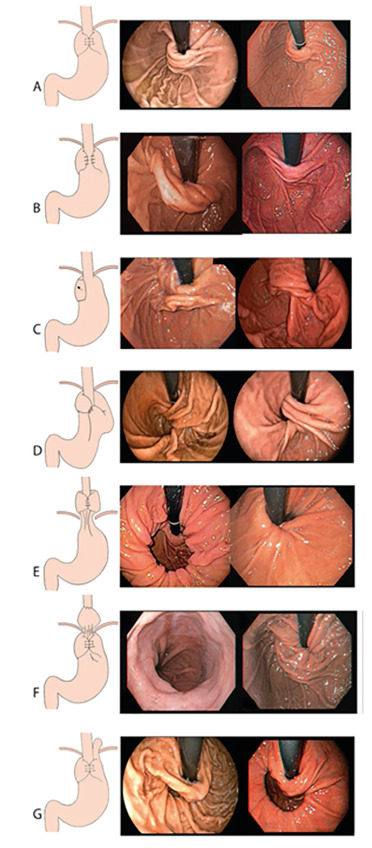
EGD Findings After Fundoplication: A) Normal Nissen, B) Partial Fundoplication, C) Disrupted Fundoplication, D) Twisted Fundoplication, E) Migrated Fundoplication, F) Slipped Fundoplication, G) Paraesophageal Hernia 2
Mnemonics
Fundoplication Variation
- Dor: Just Shutting the Front Door
- Toupet: Looks Like Balding Spot Wrapping Around the Back
- Belsey is Ballsy to Go in Through Chest
References
- Gray H. Public Domain.
- Martins BC, Souza CS, Ruas JN, Furuya CK, Fylyk SN, Sakai CM, Ide E. ENDOSCOPIC EVALUATION OF POST-FUNDOPLICATION ANATOMY AND CORRELATION WITH SYMPTOMATOLOGY. Arq Bras Cir Dig. 2021 Jan 15;33(3):e1543. (License: CC BY-4.0)