Endocrine: Hyperthyroidism
Hyperthyroidism & Diagnosis
Presentation
- Tachycardia
- Hypertension
- Palpitations & Arrhythmia
- Weight Loss
- Heat Intolerance
- Diaphoresis
- Anxiety & Fatigue
- Nausea & Vomiting
- Diarrhea
- Graves Specific Phenomenon:
- Exophthalmos
- Pretibial Myxedema
Thyroid Storm (Thyrotoxic Crisis)
- Sudden Release of Large Amounts of Thyroid Hormone
- Development is Independent of TSH Levels
- Causes:
- Cessation of Thioamide Medication
- Severe Illness
- Trauma
- Thyroid Manipulation During Surgery
- Often Have Previously Undiagnosed Graves’ Disease
- Aspirin Can Exacerbate (Decreases Protein Binding to Thyroid Hormone – More Free-T3/T4)
- High Mortality (8-25%)
- Most Common Cause of Death: High-Output Cardiac Failure
Causes
- Graves’ Disease
- Toxic Nodules
- Solitary Toxic Nodule
- Toxic Multinodular Goiter (Plummer Disease)
- Jod-Basedow Phenomenon – Patient with Iodine Deficiency Suddenly Given Excess Iodine
- Thyroiditis or “Hashitoxicosis” – Initial Hyperthyroidism Seen Prior to Development of Hypothyroidism
- Amiodarone-Induced Thyrotoxicosis (AIT) – Type 1
- Excess Exogenous Hormone Administration (Iatrogenic or Factitious)
Diagnosis
- Initial Test: TSH (Low) & Free T4/T3
- TSH Has the Highest Sensitivity & Specificity
- Next Step: Thyroid Receptor Antibodies, US and/or Radioactive Iodine Scan
- Radioactive Iodine Scan:
- High Diffuse/Symmetric Uptake: Graves’ Disease
- High Asymmetric Uptake/Multiple Hot Nodules: Toxic Multinodular Goiter
- High Uptake in Single Hot Nodule: Solitary Toxic Nodule
- Minimal/No Uptake: Thyroiditis, Iodine-Induced or Excess Exogenous Hormone Administration
- Suspicious or Nonfunctioning Nodules Require FNA

Exophthalmos 1
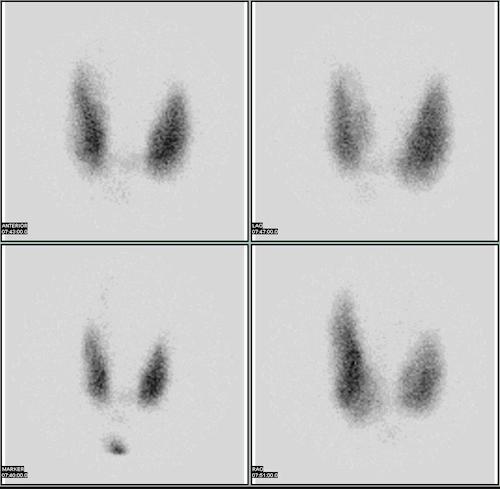
Thyroid Scan 2
Graves’ Disease
Pathophysiology
- Autoimmune Induced Production of Thyroid Hormone
- Anti-TSH Receptor IgG Ab
- Most Common Cause of Hyperthyroidism
- Causes Diffuse Symmetrical Enlargement
Treatment
- Immediate Control of Symptomatic Thyrotoxicosis: β-Blockers
- First-Line Management: Thioamides or Radioactive Iodine (RAI)
- If Primarily Treating with Thioamides – Treat for 12-18 Months
- If Fails: Consider RAI or Thyroidectomy
- If Primarily Treating with Thioamides – Treat for 12-18 Months
- Indications for Total/Near-Total Thyroidectomy:
- Suspicious Nodule (Most Common Reason)
- Noncompliant with Medication
- Planning Pregnancy in < 6 Months
- Other Indications for Cervical Surgery (Compressive Goiter, Parathyroidectomy, etc.)
- Low RAI Uptake
- Medication or RAI Failure
- Moderate-Severe Orbitopathy
Toxic Nodules
Solitary Toxic Nodule/Adenoma
- Focal Hyperplasia of Thyroid Follicular Cells Independent of TSH
- May Have TSH-Receptor Mutations that Increase Activation in Absence of TSH
- Not Associated with Iodine Intake
- Most Common in Women
Toxic Multinodular Goiter (Plummer Disease)
- Diffuse Hyperplasia of Thyroid Follicular Cells Independent of TSH
- Decreased TSH Causes Atrophy in Other Areas of the Thyroid
- Variations Cause Multiple Nodules
- Second Most Common Cause of Hyperthyroidism
- More Common in Areas with Low Iodine Intake
- Most Common in Women
Treatment
- Immediate Control of Symptomatic Thyrotoxicosis: β-Blockers
- First-Line Management: Surgery or Radioactive Iodine (RAI)
- Surgery is Generally Preferred Unless Contraindicated (High-Risk, Elderly or Frail)
- May Consider Conservative Management Only if Asymptomatic with Subclinical Hyperthyroidism
- Antithyroid Medications are Generally Not Used for Toxic Nodules Unless Pregnant to Bridge for Surgery After Delivery
Treatment
Antithyroid Medications (Thioamides)
- Methimazole
- Mechanism: Inhibits TPO
- Generally the First-Line Choice Due to Hepatotoxicity of PTU
- Contraindications: Pregnancy (Risk Cretinism)
- May Be Safe in Second/Third Trimester After Organogenesis
- Side Effects: Agranulocytosis
- Propylthiouracil (PTU)
- Mechanism: Inhibits TPO & Peripheral Conversion of T4 to T3
- Safe in Pregnancy Mn
- Side Effects: Hepatotoxic & Agranulocytosis
- Exophthalmos is Resistant to Thioamide Treatment
β-Blockers
- Reduce Sympathetic Hyperactivity
- Decrease Peripheral Conversion of T4 to T3
- Used for Immediate Control of Symptomatic Thyrotoxicosis
Radioactive Iodine (RAI)
- Sodium Iodide-131 (131I)
- RAI is Taken into Thyroid Hormone Causing Ionizing Destruction of Thyroid Follicular Cells
- Consider Pre-Treatment with Thioamides & β-Blockers to Prevent Transient Exacerbation
- Must Stop Thioamides 2-3 Days Before Treatment & Hold 2-3 Days After to Allow RAI Uptake
- Contraindications:
- Thyroid Malignancy
- Pregnancy
- Lactation
- Children < 5 Years Old
- Moderate-Severe Orbitopathy/Exophthalmos (May Worsen)
- Side Effects:
- Transient Hyperthyroidism Exacerbation
- Neck Pain
- Sialoadenitis
Thyroidectomy
- Procedure:
- Graves’ Disease: Total/Near-Total Thyroidectomy
- Solitary Toxic Nodule: Lobectomy
- Toxic Multinodular Goiter: Total/Near-Total Thyroidectomy
- Preoperative Antithyroid Medication:
- Preoperative Euthyroid State Can Prevent Thyroid Storm
- Indications:
- Graves’ Disease: All Patients Should be Made Euthyroid Preoperatively
- Toxic Nodules: Only Patients at High-Risk for Complications of Persistent Hyperthyroidism (Elderly or Cardiovascular Disease)
- Approach:
- Thioamides, β-Blocker & Potassium Iodide for 7-14 Days Preoperatively
- Lugol’s Solution (Saturated Solution of Potassium Iodide/SSKI)
- Wolff-Chaikoff Effect: High Dose Iodine Inhibits TSH
- Also Decreases Intraoperative Blood Loss (Debated & Recently Questioned)
- Generally Only Used in Graves’ Disease, Not Toxic Nodules
- During Pregnancy:
- Used Only if Antithyroid Medication First Failed or Contraindicated
- Best Time: Second Trimester
- First Trimester: Risk Fetal Development
- Third Trimester: Risk Preterm Labor
Mnemonics
Antithyroid Medications (Thioamides) in Pregnancy
- P-P: PTU is Safe in Pregnancy
References
- OpenStax College. Wikimedia Commons. (License: CC BY-SA-4.0)
- Han M. Wikimedia Commons. (License: CC BY-SA-3.0)