Pediatric Surgery: Intestinal Atresia
Duodenal Atresia
Basics
- Blockage Due to Duodenal Malformation
- Cause Complete (81%) or Partial (19%) Obstruction
- Most Common (85%) at the Junction of First/Second Portions
- Most Common Cause of Duodenal Obstruction in Newborns < 1 Week
Cause
- Cause: Failure of Recanalization
- Normal Development
- Week 6-7: Occlusion as Epithelium Proliferates
- Week 8-10: Patency Restored
Associations
- Half (55%) Have Other Congenital Anomalies
- Down Syndrome (28.2% – Most Common)
- Annular Pancreas (23.1%)
- Congenital Heart Disease (22.6%)
- Malrotation (19.7%)
- Esophageal Atresia (8.5%)
Types
- Type 1 (92%) – Obstructing Septum/Web of Mucosa & Submucosa
- Intact Muscularis, Bowel Wall & Mesentery
- Type 2 (1%) – A Short Fibrous Cord Connects Two Blind Ends
- Intact Mesentery
- Type 3 (7%) – No Connection Between Two Blind Ends with a V-Shaped Mesenteric Defect
Presentation
- Bilious Emesis
- Abdomen Nondistended – May See Upper Abdominal Fullness
- Results in Microcolon
- Maternal Polyhydramnios
Diagnosis
- Prenatal US
- Abdominal XR – Classic “Double Bubble”
- May Require Injection of 30-60 cc Air to Demonstrate Double Bubble
- No Distal Gas
- Upper GI Study – Required to Rule Out Malrotation/Volvulus
Treatment
- Initial Management: NG/OG Tube Decompression, IV Fluids & TPN
- Echocardiogram First to Rule out Cardiac Defects
- Definitive Management: “Diamond” Duodenoduodenostomy
- If Obstruction Due to Only A Thin Web: Consider Web Excision Rather than Bypass
- If Proximal Bowel is Severely Dilated: Consider Tapering Duodenoplasty
- Faster Return of Normal Peristalsis
- If Duodenum-Duodenum Anastomosis Anatomically Unfeasible: Duodenojejunostomy (#2) or Gastrojejunostomy (#3)
Diamond Duodenoduodenostomy
- Incisions:
- Proximal Transverse Incision (More Dilated)
- Distal Longitudinal Incision
- Midpoints of Each Incision Joined to the Endpoints of the Other
- Keeps Itself Patent to Allow Earlier Transit
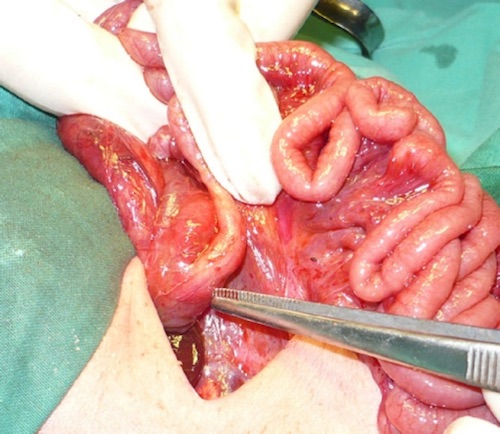
Duodenal Atresia 1

Duodenal Atresia, “Double Bubble” on XR 2
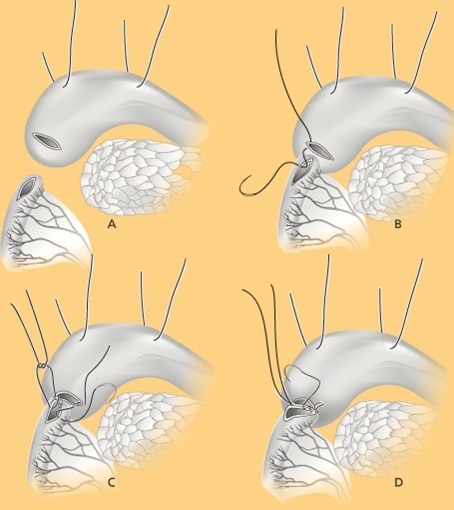
Diamond Duodenoduodenostomy 3
Jejunoileal Atresia
Basics
- Most Common Site of Atresia
- Most Common Congenital Anomaly of the Small Intestine
- 25-35% Have Other Congenital Anomalies
- Less Common Than Duodenal Atresia
- Most Are a Single Event Although 6-20% Have Multiple Atresias
- Risk for Dysfunctional Proximal Peristalsis
- Due to Intestinal Smooth Muscle Hypertrophy, Hypoplasia of Intramural Nerves & Decreased Number of Interstitial Cells of Cajal
- Most Common Cause of Early Death: Infection (PNA/Peritonitis/Sepsis)
Cause
- Cause: Intrauterine Vascular Accidents
- Risk Factors:
- Cocaine
- Pseudoephedrine
- Ergotamine Tartrate or Caffeine in Management of Migraines
Presentation
- Bilious Emesis
- Abdomen Distended
- Failure to Pass Meconium
- Results in Microcolon
- Maternal Polyhydramnios
- Jaundice

Jejunal Atresia 4
Types
- Louw & Barnard Classification:
- Type I (19%) – Mucosal Atresia (Intact Muscularis, Bowel Wall & Mesentery)
- Type II (31%) – Blind Ends (Intact Mesentery)
- Type III (46%) – Blind Ends with V-Shaped Mesenteric Defect
- Contemporary Classification:
- Type I: Mucosal Atresia (Intact Muscularis, Bowel Wall & Mesentery)
- Type II: Blind Ends (Intact Mesentery)
- Type IIIa: Blind Ends with V-Shaped Mesenteric Defect
- Type IIIb: Apple-Peel/Christmas-Tree Atresia
- Type IV: Multiple Atresias
Diagnosis
- Prenatal US
- Better at Detecting Proximal Atresia Than Distal
- Abdominal XR
- Upper GI Study
Treatment
- Initial Management: NG/OG Tube Decompression, IV Fluids & TPN
- Definitive Management: End-to-End Anastomosis
- Resect the Distal End of the Proximal Segment (Smooth Muscle Hypertrophy & Decreased Interstitial Cells of Cajal Cause a Functional Obstruction)
- Side-to-Side Risks Functional Obstruction & Blind Loop Syndrome
- Options if Large Size Difference Occurs:
- Larger End: Tapering Enteroplasty
- Smaller End: Cheatle Slit (Longitudinal Incision on Antimesenteric Border for Wider Anastomosis)
- If Concerned for Short Bowel Syndrome: Consider G-Tube Placement
References
- Mirza B, Sheikh A. Multiple associated anomalies in patients of duodenal atresia: a case series. J Neonatal Surg. 2012 Apr 1;1(2):23. (License: CC BY-3.0)
- Klinikum Stuttgart KO. Wikimedia Commons. (License: CC BY-SA-3.0)
- van der Zee DC. Laparoscopic repair of duodenal atresia: revisited. World J Surg. 2011 Aug;35(8):1781-4. (License: CC BY-NC-2.0)
- Federici S, Sabatino MD, Domenichelli V, Straziuso S. Worst Prognosis in the “Complex” Jejunoileal Atresia: Is It Real? European J Pediatr Surg Rep. 2015 Jun;3(1):7-11. (License: CC BY-NC-SA-4.0)