Small Intestine: Intestinal Failure
Intestinal Failure
Definition
- Inability of the Gut to Absorb the Necessary Water, Nutrients & Electrolytes to Sustain Life
- In the Past was Uniformly Lethal, Now Much Improved Prognosis with 90% Long-Term Survival
Causes
- Short Gut Syndrome (Most Common Cause)
- 80% of Adults
- 50% of Peds
- Adult Causes:
- Mesenteric Ischemia
- Crohn’s Disease
- Volvulus
- Chronic Intestinal Pseudo-Obstruction
- Familial Polyposis
- Tumors
- Radiation Enteritis
- Bariatric Surgery
- Pediatric Causes:
- Intestinal Atresia
- Necrotizing Enterocolitis
- Gastroschisis
- Volvulus
- Hirschsprung’s Disease with Significant Involvement of Small Intestine
- Microvillus Atrophy
- Autoimmune Enteropathy
- Intestinal Epithelial Dysplasia
Short Gut Syndrome (SGS) (Short Bowel Syndrome/SBS)
- Definition: Intestinal Failure After Extensive Loss of Small Intestine
- Defined by Function, Not Length
- Most Often from One Single Large Resection (75%), Rather than Multiple Sequential Surgeries
Bowel Length
- Residual Small Bowel < 180 cm are at Risk
- Decreased Risk: Functional Ileocecal Valve or ≥ 50% of Colon
- Jejunum Resection Better Tolerated than Ileum
- General Requirements to Survive off TPN:
- 75 cm Small Bowel without Competent Ileocecal Valve
- 50 cm Small Bowel with Competent Ileocecal Valve
Intestinal Adaptation
- Bowel Adapts Over 1-2 Years After Loss
- Most Prominent Throughout Ileum
- Structural Adaptations:
- Remnant Bowel Dilation & Elongation
- Villus Lengthening
- Microvillus Expansion
- Crypt Cell Hyperplasia
- Functional Adaptations:
- Increased Absorption/Permeability
- Increased Gut Hormonal Secretion
- Slowed Rate of Gut Transit
- Gut Microbiota Changes
Presentation
- Symptoms:
- Fatigue
- Weight Loss
- Nausea & Vomiting
- Diarrhea
- Steatorrhea
- Complications:
- Nutritional Deficiencies
- Esophagitis & Peptic Ulcers
- Cholestasis & Cholelithiasis
- Osteomalacia
- Nephrolithiasis
Diagnosis
- Clinical Diagnosis
- Supportive Tests:
- Labs – Electrolytes, Vitamin Levels & Albumin
- D-Xylose Absorption Test
- D-Xylose (Easily Absorbed Monosaccharide) Given Orally & Urine Level is Measured
- Low Urine Level Indicated Malabsorption
- Sudan III Stain Test
- Sudan Dye (High Affinity for Lipids) Used on Stool Sample to Determine Level of Fecal Fat
- High Level of Fecal Fat Indicates Steatorrhea
- Schilling Test
- Vitamin B12 Given Orally & Urine Level is Measured
- Multiple Stages with Intrinsic Factor, ABX & Pancreatic Enzymes
- Low Urine Level Indicates Malabsorption
- Vitamin B12 Given Orally & Urine Level is Measured
- Serum Citrulline Test
- Citrulline (Nonessential Amino Acid Produced by Enterocytes) Blood Level Measured
- Strong Marker for Enterocyte Mass & Low Level (< 20 μmol/L) Associated with Intestinal Failure
Intestinal Failure – Management
Initial Treatment
- Early Enteral Feeding – Vital for Intestinal Function & Adaptation
- Electrolyte Management & Parenteral Nutrition as Indicated
- PPI or H2 Blocker – Prevent Gastric Hypersecretion
- Antidiarrheal Medications as Needed
Pharmacologic Adjuncts
- GLP-1 Analog (Liraglutide)
- Supports Intestinal Epithelium
- GLP-2 Analog (Teduglutide)
- Supports Intestinal Epithelium & Adaptive Response
- Promotes Weaning from Parenteral Nutrition
- Growth Hormone & Glutamine (Enterocyte Energy Source)
- Improves Intestinal Absorption
- Glutamine Alone Does Not Appear to Benefit
- Octreotide
- Increases Transit Time & Reduces Fluid Loss
Surgical Management
- Indication: If Fails to Wean Off Parenteral Nutrition
- Restore Intestinal Continuity if Any Segments Were Previously Bypassed or Unused
- If Intestine Lengthening Necessary: Serial Transverse Enteroplasty
- Requires Dilated Bowel of Adequate Length
- If Not Dilated May Consider Segmental Reversal (Interposition of Reversed Segments to Slow Transit)
- Intestinal Transplant
- Indications:
- Lifelong Parenteral Nutrition Dependent with Irreversible Parenteral Nutation Complications
- Lifelong Parenteral Nutrition Dependent with Failure to Manage Hydration/Nutrition
- Definitions:
- Intestinal Transplant – Can Include Intestines, Liver & Multi-Visceral Transplants
- Isolated Intestinal Transplant – Only Intestines Transplanted
- Exact Operation Tailored to the Patient
- Liver-Inclusive Transplant Has Improved Survival Over Isolated Intestine Transplant Due to Immunologic Tolerance from the Liver
- Indications:
Autologous Intestinal Reconstruction Surgery (AIRS)
- Requires Dilated Bowel of Adequate Length
- Serial Transverse Enteroplasty (STEP Procedure)
- Fire Transverse Staple Loads Partially Across the Lumen Alternating from the Mesenteric & Antimesenteric Edges of Dilated Bowel
- Longitudinal Intestinal Lengthening & Tailoring (LILT/Bianchi Procedure)
- Vascular Tunnel Created Between the Mesenteric Vessels & Longitudinal Division of the Intestine into Two Separate Pieces Which are Then Anastomosed
- The First Original Intestinal Lengthening Procedure
- Fallen Out of Favor – More Complex & Risk for Compromised Blood Flow
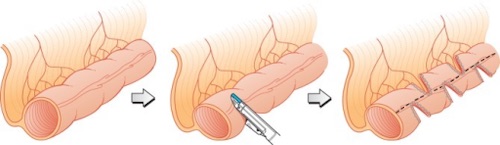
Serial Transverse Enteroplasty (STEP) 1
References
- Wester T, Borg H, Naji H, Stenström P, Westbacke G, Lilja HE. Serial transverse enteroplasty to facilitate enteral autonomy in selected children with short bowel syndrome. Br J Surg. 2014 Sep;101(10):1329-33. (License: CC BY-NC-ND-3.0)