Trauma: Liver Trauma
Liver Trauma
Grade I 2

Grade II 2

Grade III 3

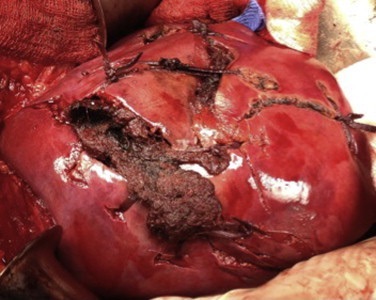
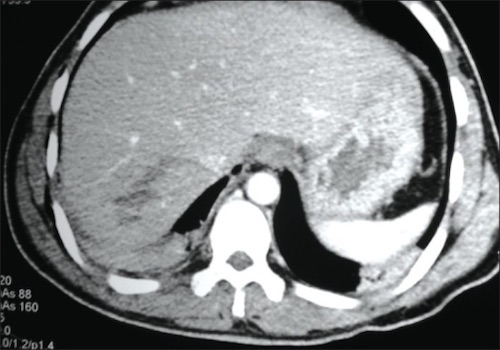
Grade IV 4

Grade V 5
Initial Management
- Unstable: Laparotomy
- Diffuse Peritonitis Indicates Bowel Injury & Warrants Laparotomy – Diffuse Peritonitis Should Never be Attributed to Solid Organ Injury as Isolated Hemoperitoneum Should Not Cause Diffuse Peritoneal Irritation
- Transient Responder: Angioembolization
- Stable: CT
- Active Extravasation or Pseudoaneurysm: Angioembolization (93% Success Rate)
- Nonoperative Management Otherwise (< 10% Failure Rates)
- If Angioembolization Fails: Laparotomy
Nonoperative Management Complications
- Early: Hemorrhage & Abdominal Compartment Syndrome
- Late: Biliary (Biloma/Fistula) & Infection (Perihepatic Sepsis/Abscess)
Liver Trauma – Surgical Management
Exposure
- Divide Falciform Ligament – Visualize Superior or Lateral Aspects
- Divide Triangular Ligaments – Further Mobilize the Right/Left Lobes
- If Stable Hematoma Noted Within Triangular Ligament: Do Not Enter
- Concern for Hepatic Vein or IVC Injury
- If Stable Hematoma Noted Within Triangular Ligament: Do Not Enter
Achieving Initial Surgical Hemostasis
- Initial: Manual Compression Until Resuscitated
- *Most Liver Bleeding is Venous
- If Significant Hemorrhage After Release: Pringle Maneuver
- 85% Success in Complex Injuries
- Up to 75 Minutes Without Adverse Sequelae
- Failure Raises Concern for Hepatic Vein/IVC Injury
- Options if Still Bleeding After Pringle Maneuver:
- Total Hepatic Isolation – Involves Pringle Maneuver, Infrahepatic IVC Occlusion & Suprahepatic IVC Occlusion
- Also Consider Supraceliac Aortic Occlusion – Abdominal Blood Flow Will Be Lost from Circulation Above the Diaphragm
- Atriocaval (Schrock) Shunt
- Total Hepatic Isolation – Involves Pringle Maneuver, Infrahepatic IVC Occlusion & Suprahepatic IVC Occlusion
Atriocaval (Schrock) Shunt
- Consider for Retrohepatic Venous Injury
- Shunt from IVC to Right Atrium
- Technique:
- Pringle Maneuver
- Median Sternotomy
- Prepare Shunt
- Chest Tube – Cut a Hole 20 cm from the Nearest Drainage Hole
- Endotracheal Tube – Cut a Hole 17-18 cm from the Nearest Hole Past the Balloon
- Control Perihepatic IVC with Rumel Tourniquets:
- Control Suprarenal IVC (Omit Step if Using an ETT)
- Control Intrapericardial IVC
- Insert the Shunt Through a Right Atrial Incision
- Apply a Partially Occluding Clamp on the Right Atrial Appendage
- Place a Purse-String Suture
- Create an Incision Between the Purse-String
- Remove the Clamp
- Insert the Shunt Through the Incision
- Palpate the Tube terminating in the Correct Infrarenal Position
- All Shunt Holes Should Be Outside the Area of Vascular Isolation
- Secure all Purse-Strings, Tourniquets or Inflated Balloons
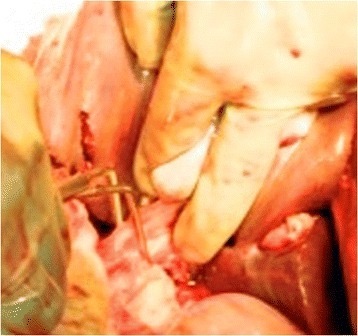
Pringle Maneuver 6
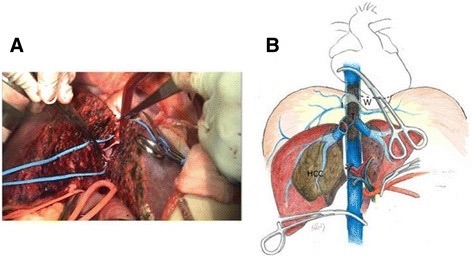
Total Hepatic Isolation 7
Surgical Treatment
- Subcapsular Hematoma: Leave
- Minor Injuries (Grade I-II)
- Initial: Simple Techniques
- Techniques:
- Manual Compression (5-10 Minutes)
- Topical Agents (Fibrin Glue/Surgicel)
- Electrocautery/Argon Beam Electrocoagulation
- If Successful – No Further Intervention
- No Drain Needed if No Obvious Bile Leakage
- Techniques:
- Superficial Laceration: Suture Hepatorrhaphy
- Liver Suture (Absorbable & Blunt Tipped Needle)
- Deep Laceration: Omental Packing & Loosely Approximate Edges
- Initial: Simple Techniques
- Complex Injuries (Grade III-V): Hepatectomy
- Finger Fracture Technique
- Glisson’s Capsule Incised Towards Injury
- Parenchyma Fractured Between Thumb and Forefinger
- Rapidly Exposes Lacerated Vessels and Bile Ducts for Direct Ligation/Repair
- Debride Devascularized Tissue Once Hemostasis Achieved
- Consider Omental Pedicle Packing
- Leave Closed-Suction Drains
- Finger Fracture Technique
- Juxtahepatic Venous Injury (Grade V): Perihepatic Packing
- If Controlled – No Further Intervention Indicated
- Consider Endovascular Stent When Stable Before Packing Removal
- Other Options:
- Direct Hepatectomy (Finger Fracture Through Cantlie’s Line) to Reach Injury
- Venovenous Bypass with Vascular Exclusion & Primary Repair
- Last Resort: Total Hepatectomy & Delayed Liver TXP
- Damage Control: Perihepatic Packing & Planned Reexploration
Portal Triad Injury
- CBD Injury
- < 50% Circumference: Primary Repair (Over T-Tube)
- > 50% Circumference: Roux-en-Y Hepaticojejunostomy
- Delayed Biloma: Percutaneous Drain
- Portal Vein Injury: Lateral Venorrhaphy
- If Emergent: Portal Vein Ligation
- May Require Pancreas Neck Division to Access
- Hepatic Artery Injury: Ligation
- Concurrent Cholecystectomy Mandatory
- Increased Risk for Hepatic Abscess
Mnemonics
Liver Injury Grading
- I/II/III: 1/2/3 cm Depth
References
- Latifi R, Khalaf H. Selective vascular isolation of the liver as part of initial damage control for grade 5 liver injuries: Shouldn’t we use it more frequently? Int J Surg Case Rep. 2015;6C:292-5. (License: CC BY-NC-SA-3.0)
- Parray FQ, Wani ML, Malik AA, Thakur N, Wani RA, Naqash SH, Chowdri NA, Wani KA, Bijli AH, Irshad I, Nayeem-Ul-Hassan. Evaluating a conservative approach to managing liver injuries in Kashmir, India. J Emerg Trauma Shock. 2011 Oct;4(4):483-7.(License: CC BY-NC-SA-3.0)
- Ghnnam WM, Almasry HN, Ghanem MA. Non-operative management of blunt liver trauma in a level II trauma hospital in Saudi Arabia. Int J Crit Illn Inj Sci. 2013 Apr;3(2):118-23. (License: CC BY-NC-SA-3.0)
- Zago TM, Tavares Pereira BM, Araujo Calderan TR, Godinho M, Nascimento B, Fraga GP. Nonoperative management for patients with grade IV blunt hepatic trauma. World J Emerg Surg. 2012 Aug 22;7 Suppl 1(Suppl 1):S8. (License: CC BY-2.0)
- Tugnoli G, Cinquantini F, Coniglio C, Biscardi A, Piccinini A, Gordini G, Di Saverio S. “The best is nothing”: Non-operative management of hemodynamically stable grade V liver trauma. J Emerg Trauma Shock. 2015 Oct-Dec;8(4):239-40.(License: CC BY-NC-SA-3.0)
- Coccolini F, Montori G, Catena F, Di Saverio S, Biffl W, Moore EE, Peitzman AB, Rizoli S, Tugnoli G, Sartelli M, Manfredi R, Ansaloni L. Liver trauma: WSES position paper. World J Emerg Surg. 2015 Aug 25;10:39. (License: CC BY-4.0)
- Ho MH, Chen TW, Ou KW, Yu JC, Hsieh CB. Rescue strategy for advanced liver malignancy with retrohepatic inferior vena cava thrombi: experience to promote surgical oncological benefit. World J Surg Oncol. 2017 Apr 12;15(1):83. (License: CC BY-4.0)