Oncology: Lymphoma
Lymphoma
Definition
- Definition: Cancer of Lymphocytes
- Often Considered a Cancer of Lymph Nodes
- Classification:
- Hodgkin’s Lymphoma (HL) – Presence of Reed-Sternberg Cells
- Non-Hodgkin’s Lymphoma (NHL) – Does Not Contain Reed-Sternberg Cells
Hodgkin’s Lymphoma (HL)
- Less Common Type
- Younger Patient Population – Median Age is 39
- 86% 5-Year Survival
- Cell Types:
- Reed-Sternberg Cells – Large Mutated B Lymphocytes
- Appearance of “Owl’s Eye” Nuclei
- Popcorn Cells – Variant of Reed-Sternberg Cells
- Appearance of “Popcorn”
- Also Called Lymphocytic & Histiocytic (L&H) Cells
- Reed-Sternberg Cells – Large Mutated B Lymphocytes
- Subtypes (5):
- Classical Hodgkin’s Lymphoma (90%) – Presence of Reed-Sternberg Cells
- Nodular Sclerosis Classical Hodgkin’s Lymphoma
- Mixed Cellularity Classical Hodgkin’s Lymphoma
- Lymphocyte-Rich (Best Prognosis)
- Lymphocyte-Depleted (Worst)
- Nodular Lymphocyte-Predominant Hodgkin’s Lymphoma (10%) – Presence of Popcorn Cells
- Classical Hodgkin’s Lymphoma (90%) – Presence of Reed-Sternberg Cells
Non-Hodgkin’s Lymphoma (NHL)
- Most Common Type
- Older Patient Population – Median Age is 66
- 70% 5-Year Survival
- Subtypes (> 60):
- B-Cell Lymphoma (85% – Most Common):
- Diffuse Large B-Cell Lymphoma (DLBCL) – Most Common Subtype
- Follicular Lymphoma
- Mantle Cell Lymphoma
- Marginal Zone Lymphoma
- Burkitt Lymphoma
- Many Others
- T-Cell Lymphoma (15%):
- T-Lymphoblastic Lymphoma
- Peripheral T-Cell Lymphoma
- Many Others
- B-Cell Lymphoma (85% – Most Common):
Primary Gastrointestinal (GI) Lymphoma
Presentation
- Variable/Diffuse Lymphadenopathy
- Constitutional Symptoms (Fever, Night Sweats, Weight Loss)
- Hepatosplenomegaly
- NHL is the Most Common Cause of Splenomegaly
- Nausea & Vomiting
- Most Common Cause of Chylous Ascites
Diagnosis
- Gold Standard Work-Up: Excisional Bx
- *Core Needle Biopsy May Be Sufficient in Diagnosing Cancers with Metastasis to Nodes
- FNA is Inadequate Exclude the Diagnosis or Make a Definitive Classification
- Generally Need to Excise a Node & Send it Fresh for Flow Cytometry
- Usually Try to Sample Nodes that are Easiest to Access with Lower Chance of Complications Such as Axillary or Inguinal Nodes
Diagnostic Yield of Palpable Nodes
- Overall Yield: 70.4%
- Supraclavicular: 90% – Highest Yield
- Cervical: 76.4%
- Axillary: 62.5%
- Inguinal: 38.5% – Lowest Yield
Staging (Lugano Classification)
- Stage I – Involvement of a Single Lymph Node Region
- IE – Involvement of a Single Extralymphatic Organ/Site without Nodal Involvement
- Stage II – Involvement of ≥ 2 Lymph Node Regions on the Same Side of the Diaphragm
- IIE – Also Involves Limited Contiguous Extralymphatic Organs/Tissue
- Stage III – Involvement of Lymph Node Regions on Both Sides of the Diaphragm
- Stage IV – Diffuse/Disseminated Disease which Involves Noncontiguous Extralymphatic Organs/Tissue (Bone Marrow/Liver/Lung)
- May or May Not Involve Lymph Nodes
Treatment
- Primary Treatment: Chemotherapy

Facial Burkitt Lymphoma 1
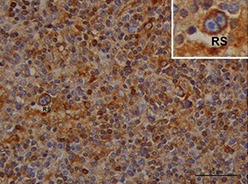
Reed-Sternberg Cells 2
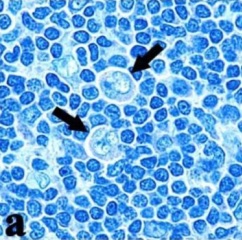
Popcorn Cells 3
References
- Blyth M. Wikimedia Commons. (License: CC BY-SA-2.5)
- Caocci G, Greco M, Fanni D, Senes G, Littera R, Lai S, Risso P, Carcassi C, Faa G, La Nasa G. HLA-G expression and role in advanced-stage classical Hodgkin lymphoma. Eur J Histochem. 2016 Apr 11;60(2):2606. (License: CC BY-NC-3.0)
- Agostinelli C, Pileri S. Pathobiology of hodgkin lymphoma. Mediterr J Hematol Infect Dis. 2014 Jun 5;6(1):e2014040. (License: CC BY-2.0)