Breast: Mastitis & Abscess
Mastitis & Abscess
Definitions
- Mastitis: Mammary Gland Inflammation
- Lactational (Puerperal) Mastitis: Mastitis Associated with Breastfeeding (Most Common)
- Most Common in the First Three Months
- Periductal Mastitis (Ductal Ectasia): Inflammation of the Subareolar Ducts with Ductal Dilation, Obstruction & Filling with Fluid
- Usually Causes a Chronic Inflammation
- Lactational (Puerperal) Mastitis: Mastitis Associated with Breastfeeding (Most Common)
- Breast Abscess: Purulent Fluid-Filled Cavity of the Breast
Microbiology
- Staphylococcus aureus – Most Common Organism
- Other Organisms:
- Streptococci
- Enterococci
- Bacteroides
Causes
- Lactational Mastitis:
- Partial Duct Blockage
- Milk Overproduction
- Infrequent Feedings
- Rapid Weaning
- Nipple Trauma
- Periductal Mastitis (Ductal Ectasia):
- Not Entirely Certain
- Obstruction – Debated
- Risk Factors: Smoking & Piercings
- Breast Abscess
- Primary: No Inciting Disease
- Secondary: Preexisting Mastitis or Cellulitis
Presentation
- Pain
- Swelling
- Erythema
- Fever
- Periductal Mastitis Can Cause Green-Brown Creamy Nipple Discharge (Most Common Cause)
- Abscess Can Have a Palpable Fluctuant Mass
Diagnosis
- Clinical Diagnosis
- May Consider Breast Milk Culture to Guide Antibiotic Therapy
- Consider US to Evaluate for Abscess if Fails to Improve Over 48-72 Hours
Treatment
- Mastitis:
- Initial Treatment: NSAID’s & Cold Compress
- If Infective/Beyond 12-24 Hours: Antibiotic Therapy
- Primary Antibiotics: Dicloxacillin or Cephalexin
- Consider Amoxicillin-Clavulanate (Augmentin) for Periductal Mastitis
- If at Risk for MRSA: Trimethoprim-Sulfamethoxazole (TMP-SMX/Bactrim)
- If Severe or Systemic: IV Vancomycin
- Primary Antibiotics: Dicloxacillin or Cephalexin
- Continue Feeding & Promote Complete Emptying (Pumping or Hand Expression if Needed)
- Abscess: Antibiotics & Drainage
- Antibiotics: Similar to Mastitis
- Drainage:
- Preferred Method: Needle Aspiration (Most Resolve After 2-3 Aspirations)
- I&D Can Cause Mammary Duct Fistula or Milk Fistula
- Indications for Incision & Drainage (I&D):
- Refractory
- Multiloculated
- Recurrent Abscess
- Skin Compromised (Ischemia or Necrosis)
- Preferred Method: Needle Aspiration (Most Resolve After 2-3 Aspirations)
- Continue Feeding & Promote Complete Emptying
- Although Bacteria are Present in Milk, No Harm is Done to the Infant
- If Too Painful: Consider Pumping or Hand Expression with Feeding on the Unaffected Side
- If Treatments Continue to Fail: Consider Skin Biopsy for Inflammatory Breast Cancer

Mastitis 1
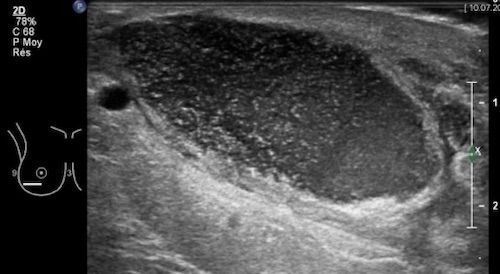
Breast Abscess on US 2
Granulomatous Mastitis
Basics
- Definition: Rare Benign Inflammatory Disease of the Breast Causing Granulomas
- Causes:
- Idiopathic – May Be Associated with Corynebacterium kroppenstedtii
- Tuberculosis (TB)
- Sarcoidosis
Presentation
- Peripheral Inflammatory Breast Mass
- May Have Abscess or Overlying Skin Inflammation/Ulceration
Diagnosis
- Initial Imaging: US
- Diagnosis: Core Needle Biopsy (CNB)
- Pathology: Non-Necrotizing Granulomatous Lesions Centered on a Breast Lobule
- Send for Acid-Fast Stains & Culture (Rule Out TB)
Treatment
- Primary Treatment: Conservative Management
- Treat Mastitis or Abscess as Indicated
- For Tuberculosis: Typical TB “RIPE” Antibiotic Regimen (Rifampin, Isoniazid, Pyrazinamide & Ethambutol)
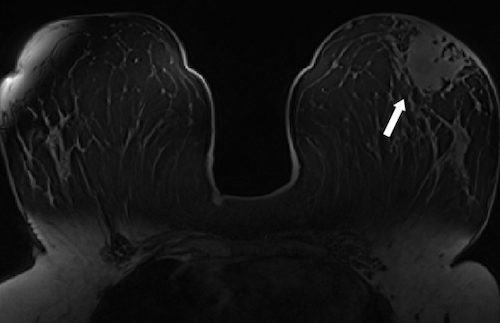
Granulomatous Mastitis on MRI 3
References
- Lut J. Wikimedia Commons. (License: CC BY-SA-4.0)
- di Summa PG, Yvon A, Larcher L, Raffoul W, Koch N. Propionibacterium avidum infection following breast reduction: high morbidity from a low-virulence pathogen. J Surg Case Rep. 2015 Feb 10;2015(2):rjv002. (License: CC BY-NC-4.0)
- Bilal A, Badar Albadar F, Bashir Barlas N. Granulomatous Mastitis: Imaging of Temporal Evolution. Scientifica (Cairo). 2016;2016:3737528. (License: CC BY-4.0)