Surgical Critical Care: Mechanical Ventilation –Airway Pressures
Airway Pressures
Pressure Gradients
- Trans-Airway Pressure = Atmospheric Pressure – Alveolar Pressure
- Trans-Thoracic Pressure = Alveolar Pressure – Body Surface Pressure
- Trans-Pulmonary Pressure = Alveolar Pressure – Pleural Pressure
- Trans-Respiratory Pressure = Atmospheric Pressure – Body Surface Pressure
- Trans-Respiratory Pressure = Trans-Airway Pressure + Trans-Thoracic Pressure
Ventilator Pressure Evaluation
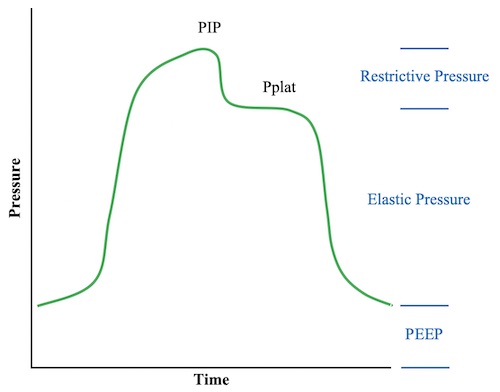
- Peak Inspiratory Pressure (PIP) – Highest Pressure Seen During Inspiration
- Maximum Acceptable PIP < 35-40 cm H2O
- Plateau Pressure (Pplat) – Static Pressure at the End of Full Inspiration
- Estimates Alveolar Pressure
- Normal Plateau Pressure < 30 cm H2O
- Measure with an “Inspiratory Hold” Maneuver on the Ventilator
- Ventilation is Held for 2 Seconds After Inspiratory Flow is Complete to Evaluate Plateau Pressure
Relationships/Equations
- PIP = PEEP + Elastic Pressure + Restrictive Pressure
- Also: PIP = Pplat + Restrictive Pressure
- Pplat = PEEP + Elastic Pressure
- Restrictive Pressure = Flow x Resistance
- Elastic Pressure = Volume x Elastance = Volume/Compliance
Compliance
- Compliance = Change in Volume / Change in Pressure
- Elastance = 1/Compliance
- Dynamic Compliance = Tidal Volume / (Elastic Pressure + Restrictive Pressure)
- Dynamic Compliance = Tidal Volume / (PIP – PEEP)
- Static Compliance = Tidal Volume / Elastic Pressure
- Static Compliance = Tidal Volume / (Pplat – PEEP)
Ventilator Pressures
Elevated Airway Pressures
Effects of High Pressure
- High Airway Pressure Itself is Not Always Harmful – Unless it is Caused by High Alveolar Pressure
- Effects of Elevated Alveolar Pressure:
- Barotrauma (Causes Acute Lung Injury & Air Leaks)
- Decreased Venous Return (Decreases Cardiac Output & Blood Pressure)
- Decreased Ventilation
Causes of High Pressures
- High Restrictive Pressure (High PIP with Normal Pplat):
- Increased Flow
- Increased Airway Resistance
- Obstructed Endotracheal Tube
- Displaced Endotracheal Tube
- Tubing or Endotracheal Kinking
- Pooling of Condensed Water in the Circuit
- Bronchospasm
- Aspiration, High Secretions or Mucous Plugging
- High Elastic Pressure (High Pplat):
- Increased Volume
- Air Trapping
- Decreased Compliance
- Decreased Lung Compliance:
- Atelectasis
- Pulmonary Consolidation
- Pulmonary Edema
- Pleural Effusion
- Pneumothorax
- Decreased Chest Wall Compliance:
- Abdominal Distention
- Morbid Obesity
- Inadequate Anesthesia
- Kyphoscoliosis
- Malignant Hyperthermia
- Patient-Ventilator Dysynchrony
- Decreased Lung Compliance:
- Increased Volume
- High PEEP
Evaluation of High Pressures of Unknown Cause
- Disconnect from Ventilator & Manually Bag the Patient if Necessary
- Can Evaluate Resistance While Bagging
- Check the Ventilator for Correct Settings
- Check the Circuit for Obstruction or Kinking
- Pass a Suction Catheter Through the Endotracheal Tube to Assess Patency/Obstruction
- Examine End-Tidal CO2
- Chest X-Ray to Check Endotracheal Tube Position & Pulmonary Pathology
- Watch for Ventilator Dyssynchrony
- Physical Examination (Wheezing or Asymmetrical Chest Expansion)
- Preform an “Inspiratory Hold” Maneuver to Differentiate Elastic from Restrictive Pressures