Surgical Critical Care: Mechanical Ventilation – Modes
Ventilator Modes
Non-Controlled Ventilation
- Continuous Positive Airway Pressure (CPAP)
- Pressure Support Ventilation (PSV)
- PSV Variations:
- CPAP with PSV (Similar to BPAP)
- Automatic Tube Compensation
- Volume Support Ventilation (VSV)
Volume-Controlled Ventilation
- Controlled Mechanical Ventilation (CMV)
- Assist-Control Ventilation (AC)
- Synchronized Intermittent Mechanical Ventilation (SIMV)
Pressure-Controlled Ventilation
- Same Modes as Volume-Controlled Ventilation (CMV, AC & SIMV)
Advanced Modes
- Airway Pressure Release Ventilation (APRV)
- High-Frequency Oscillatory Ventilation (HFOV)
- Adaptive Support Ventilation (ASV)
- Neurally Adjusted Ventilatory Assist (NAVA) Ventilation
Non-Controlled Ventilation
Modes
- Continuous Positive Airway Pressure (CPAP)
- Provides a Continuous Pressure Level (Similar to PEEP)
- No Additional Support Provided to Patient-Triggered Breaths
- All Breaths are Patient-Triggered – Patient Determines Rate & Volume
- Pressure Support Ventilation (PSV)
- Additional Pressure Support Provided to Patient-Triggered Breaths
- All Breaths are Patient-Triggered – Patient Determines Rate & Volume
- PSV Variations:
- CPAP with PSV (Similar to BPAP)
- Pressure Support is in Addition to PEEP
- PSV 10/5 Indicates 5 cm H2O of PEEP & 15 cm H2O During Support
- Automatic Tube Compensation
- Continuously Adjusts Pressure Support to the Level Needed to Overcome the Endotracheal Tube
- Volume Support Ventilation (VSV)
- Continuously Adjusts Pressure Support to the Level Needed to Achieve a Target Tidal Volume
- Newer Technique & Some Evidence Suggests Decreased Weaning Time & Total Ventilation Time
- CPAP with PSV (Similar to BPAP)
Use
- Used Primarily for Ventilator Weaning – Pressure Used to Overcome the Resistance of the Endotracheal Tube
- Disadvantages:
- Higher Work of Breathing & Can Cause Respiratory Fatigue
- Can Result in CO2 Retention & Acidosis
- Poor Choice for Full Ventilatory Support
Volume-Controlled Ventilation
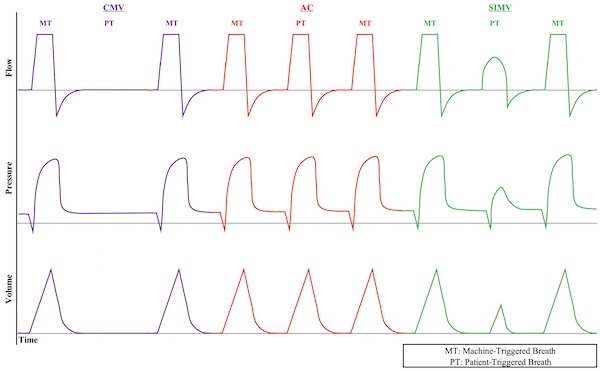
Controlled Mechanical Ventilation (CMV)
- Mechanism:
- Sets a Controlled Minute Ventilation (Rate & Volume)
- Does Not Allow Any Patient-Triggered Breaths
- Advantages:
- Lowest Work of Breathing
- Set Minute Ventilation is Easily Adjusted
- Disadvantages:
- Less Comfortable
- May See Ventilator Dyssynchrony with Wasted Effort
- May Require Deeper Sedation or Paralytics
Assist-Control Ventilation (AC)
- Mechanism:
- Sets a Minimum Minute Ventilation (Rate & Volume)
- Allows Patient-Triggered Breaths in Addition to Set Minimum Breaths
- Patient-Triggered Breaths are at the Set Volume
- Advantages:
- Increased Comfort
- Allows Sedation Weaning
- Improved Ventilator Synchrony
- Lower Work of Breathing than SIMV
- Disadvantages:
- Higher Work of Breathing than CMV
- Can Hyperventilate with “Breath-Stacking”
Synchronized Intermittent Mechanical Ventilation (SIMV)
- Mechanism:
- Sets a Minimum Minute Ventilation (Rate & Volume)
- Allows Patient-Triggered Breaths in Addition to Set Minimum Breaths
- Patient-Triggered Breaths are at a Patient’s Own Volume
- Advantages:
- May Allow Exercise of Respiratory Muscles (No Proven Evidence of Any Advantage to SIMV)
- Disadvantages:
- Higher Work of Breathing & Can Cause Respiratory Fatigue
- Less Comfortable
- Can Hyperventilate with “Breath-Stacking”
Volume-Controlled Ventilation
Pressure-Controlled Ventilation
Pressure-Controlled Ventilation
- Used Much Less Often than Volume-Controlled Ventilation
- Mechanism:
- Provides a Set Airway Pressure for Given Inspiratory Time
- Uses Inspiratory Pressure Level Instead of Tidal Volume
- Delivered Using Same Modes as Volume-Controlled Ventilation (CMV, AC & SIMV)
- Advantages:
- Peak Inspiratory Pressure (PIP) is Constant (Inspiratory Pressure + PEEP)
- Decreased Risk for Barotrauma by Lower PIP
- Increased Mean Airway Pressure & Duration of Alveolar Recruitment
- Increased Comfort & Decreased Work of Breathing
- May Allows Better Synchrony with the Ventilator
- Peak Inspiratory Pressure (PIP) is Constant (Inspiratory Pressure + PEEP)
- Disadvantages:
- Tidal Volume & Minute Ventilation is Variable
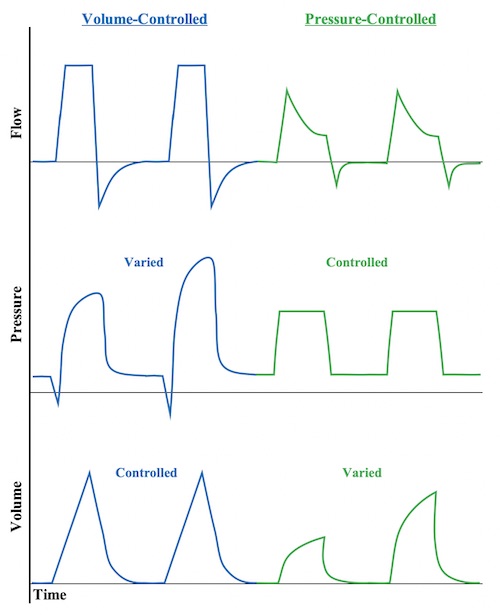
Volume- vs Pressure-Controlled Ventilation
Advanced Modes of Ventilation
Airway Pressure Release Ventilation (APRV)
- Mechanism:
- Maintains High Pressure (P High) for an Extended Time (T High) to Optimize Oxygenation
- Pressure Released (P Low) for Short Time Period of Time (T Low) to Allow Ventilation
- Longer Inspiratory/Expiratory Ratio: 80-95%
- Spontaneous Breathing is Permitted but Will Have Low Tidal Volumes at the Higher Pressures
- Most Commonly Used for Severe ARDS When Having Difficulty Oxygenating on Other Modes
- Advantages:
- Maximize Alveolar Recruitment & Oxygenation
- Lung-Protective (Lower Peak Pressures & Less Barotrauma)
- More Comfortable than CMV – Allows Decreased Sedation
- Disadvantages:
- Not Ideal if Requiring Heavy Sedation – Spontaneous Breathing is Important for Ventilation
- Generally Avoided in Severe Obstructive Airway Disease – Risks Hyperinflation with Increased Pressure & Barotrauma
- Generally Avoided for High Ventilatory Requirements
High-Frequency Oscillatory Ventilation (HFOV)
- Mechanism:
- Very High Respiratory Rate (Up to 900 Breaths per Minute) by a High-Frequency Oscillatory Pump
- Rate Set to 3-15 Hertz
- Rate is So Fast That the Airway Pressure Merely Oscillates Around a Constant Mean Airway Pressure
- Tidal Volumes are Very Small
- Very High Respiratory Rate (Up to 900 Breaths per Minute) by a High-Frequency Oscillatory Pump
- Most Commonly Used for Severe ARDS Only When Having Difficulty Oxygenating on Other Modes – Should Not Be Used Routinely (May Actually Increase Mortality)
- Advantages:
- Maintains Alveolar Recruitment & Oxygenation
- Lung-Protective (Lower Peak Pressures & Less Barotrauma)
- Disadvantages:
- Significant Discomfort & Requires Heavy Sedation or Paralysis
- Decreased Expiratory Time Creates Risk for Hyperinflation with Increased Pressure & Barotrauma
Adaptive Support Ventilation (ASV)
- Mechanism:
- Continual Adjustments are Automatically Made to Respiratory Rate and Inspiratory Pressure to Achieve a Goal Minimum Minute Ventilation (MMV)
- Optimal Settings Determined by the “Otis Equation” to Minimize Work of Breathing
- Accounts for Respiratory Mechanics (Resistance, Compliance, Dead Space – Calculated)
- Patient-Triggered Breaths are Given Pressure Support
- Pressure-Controlled Breaths are Given as Needed to Achieve a Calculated Respiratory Rate
- Continual Adjustments are Automatically Made to Respiratory Rate and Inspiratory Pressure to Achieve a Goal Minimum Minute Ventilation (MMV)
- Settings:
- Ventilate by Setting a Percentage of Minimum Volume (MinVol) of Desired Minute Ventilation
- 100% Normal, 120% in ARDS, 90% in Asthma, 110% in Others
- Add 20% for Fevers > 101.3 F
- Oxygenate by Setting PEEP and FiO2
- Ventilate by Setting a Percentage of Minimum Volume (MinVol) of Desired Minute Ventilation
- Advantages:
- Decreased Work of Breathing
- Attempts Lung Protective Strategies to Prevent Volutrauma, Barotrauma & Auto PEEP
- May Decrease Ventilator Weaning Time in COPD
Neurally Adjusted Ventilatory Assist (NAVA) Ventilation
- Mechanism:
- Catheter Implanted in a Gastric Tube Detects Electrical Discharge in the Diaphragm
- Diaphragmatic Excitation Triggers a Mechanical Breath
- The Degree of Assist Varies by the Amplitude of the Electrical Discharge
- Tidal Volume Continuously Varies
- Advantages:
- Neural-Ventilator Coupling (Time Between Spontaneous Breath & Delivered Mechanical Breath) is Faster than the Conventional Modes
- May Increase Ventilator Synchrony
- Disadvantages:
- Requires Spontaneous Breathing – Unable to Use with Heavy Sedation or Blunted Respiratory Drive