Skin & Soft Tissue: Necrotizing Soft Tissue Infection (NSTI)
Necrotizing Soft Tissue Infection (NSTI)
Definitions/Variations
- Necrotizing Soft Tissue Infection (NSTI): Necrotizing Infection of the Skin & Soft Tissue
- Most (75%) are Polymicrobial
- Most Common Monomicrobial Organism: Group A Streptococcus (GAS)
- Includes the Other Variations Below
- Necrotizing Cellulitis: Necrotizing Infection of the Skin
- Spare Fascia & Deep Muscle Compartments
- Necrotizing Fasciitis: Necrotizing Infection that Spreads Along Fascia Deep to the Subcutaneous Tissue
- Less Blood Supply Along Fascial Planes Allow More Rapid Spread of Bacteria Before Skin Changes are Seen
- Necrotizing Myositis: Necrotizing (Non-Clostridial) Infection Extending into the Deep Muscle Compartments
- Most Common Organism: Group A Streptococcus (GAS)
- Clostridial Myonecrosis (Gas Gangrene): Necrotizing Clostridial Infection Extending into the Deep Muscle Compartments
- May Not Have Cellulitis
- Most Common Organisms: Clostridium perfringens (Traumatic) & Clostridium septicum (Non-Traumatic)
- Fournier’s Gangrene: Necrotizing Infection of the Perineum
- Most are Polymicrobial
Classification of Necrotizing Fasciitis
- Clostridial Infection
- Usually Associated with Myonecrosis
- Non-Clostridial Infection
- Type I: Polymicrobial
- Type II: Monomicrobial
- Organisms: Group A Streptococcus (Most Common), Staphylococcus aureus & MRSA Mn
- Type III: Marine Bacteria (Vibrio)
- Type IV: Fungal (Candida)
Prognosis
- Rapidly Progress
- High Mortality (25%)
- Disfigurement & Disability Can Be Considerable
Risk Factors
- Trauma
- IV Drug Use
- Surgery
- Obesity
- Alcoholism
- Immunosuppression (Diabetes, Cirrhosis, HIV)
- Mucosal Brach (Hemorrhoids, Rectal Fissure)
- Malignancy
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) – Debated
Presentation
- Severe Pain (Out-of-Proportion)
- Erythema (Without Sharp Margins)
- Edema
- Bullae or Ecchymosis
- Crepitus
- From Anaerobic Production of Nitrogen/Hydrogen Not Readily Absorbed by Tissue
- Visible Skin Necrosis
- Hypoesthesia (Decreased Sensation)
- Late Finding from Small Blood Vessel Thrombosis & Superficial Nerve Destruction
- Fever
- Murky Gray (“Dishwater”) Fluid Drainage

NSTI of Abdominal Wall 1

Necrotizing Fasciitis 2

Fournier’s Gangrene 3
Diagnosis
- Diagnosis is Only Confirmed by Surgical Exploration
- Radiology – Soft Tissue Gas, Fluid Collections & Inflammatory Changes
- CT Scan is the Best Initial Imaging
- LRINEC Score
- “Laboratory Risk Indicator for Necrotizing Fasciitis”
- Factors:
- CRP:
- < 150 mg/L: 0
- ≥ 150 mg/L: +4
- WBC:
- < 15 Cells/mm3: 0
- 15-25 Cells/mm3: +1
- > 25 Cells/mm3: +2
- Hemoglobin:
- > 13.5 g/dL: 0
- 11-13.5 g/dL: +1
- < 11 g/dL: +2
- Sodium:
- ≥ 135 mmol/L: 0
- < 135 mmol/L: +2
- Creatinine:
- ≤ 1.6 mg/dL: 0
- > 1.6 mg/dL: +2
- Glucose:
- ≤ 180 mg/dL: 0
- > 180 mg/dL: +1
- CRP:
- Interpretation:
- Low Risk (0-5): < 50%
- Intermediate Risk (6-7): 50-75%
- High Risk (8-13): > 75%
- Specific but Poor Sensitivity – Should Not Be Used to Rule Out

Soft Tissue Gas on XR
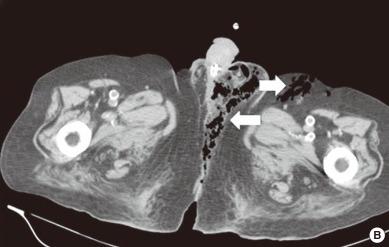
Fournier Gangrene on CT 4
Treatment
- Primary Treatment: Emergent Aggressive Surgical Debridement & Empiric Antibiotics
- May Require Repeat Debridement Every 1-2 Days
- Extremities May Require Amputation
- Treat with Serial Wet-to-Dry Dressing Changes (May Consider Using Dakin’s Solution)
- Empiric Antibiotic Regimen: Piperacillin-Tazobactam or Carbapenem Plus Vancomycin & Clindamycin
- Broad Spectrum Coverage:
- Piperacillin-Tazobactam (Zosyn)
- Meropenem (Merrem)
- Ertapenem (Invanz)
- Imipenem
- Vancomycin – Adds MRSA Coverage
- Clindamycin – Inhibits Ribosomal Exotoxin Synthesis
- Panton-Valentine Leucocidin (PVL)
- *Deescalate Based on Intraoperative Cultures
- Broad Spectrum Coverage:
- Adjunct Therapies:
- Hyperbaric Oxygen Therapy
- Intravenous Immunoglobulin (IVIG)
- Plasmapheresis
- Consider Diverting Colostomy for Severe Perineal Infections
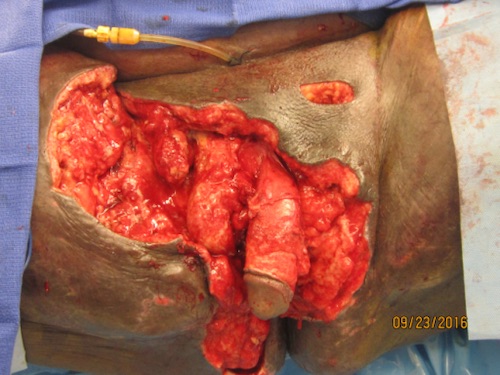
Aggressive Surgical Debridement 5
Mnemonics
Most Common Single Bacteria that Causes NSTI
- Group A Strep (GAS) is the Most Common Monomicrobial “Gas”-Forming Organism
References
- Kulkarni M, Vijay Kumar G, Sowmya G, Madhu C, Ramya S. Necrotizing soft-tissue infection: laboratory risk indicator for necrotizing soft tissue infections score. J Lab Physicians. 2014 Jan;6(1):46-9. (License: CC BY-NC-SA-3.0)
- Sadasivan J, Maroju NK, Balasubramaniam A. Necrotizing fasciitis. Indian J Plast Surg. 2013 Sep;46(3):472-8. (License: CC BY-NC-SA-3.0)
- Bakari AA, Ali N, Gadam IA, Gali BM, Tahir C, Yawe K, Dahiru AB, Mohammed BS, Wadinga D. Fistula-in-Ano Complicated by Fournier’s Gangrene Our Experience in North-Eastern Region of Nigeria. Niger J Surg. 2013 Jul;19(2):56-60. (License: CC BY-NC-SA-3.0)
- Lin WT, Hsieh CF, Chao CM. Subcutaneous Gas of the Perineal Area: Radiographic Signs of Fournier’s Gangrene.J Korean Med Sci. 2016;31(6):1007-1008. (License: CC BY-NC-4.0)
- Smith MT Jr, Graham JN Jr, Levy EB, Olugbade K, Flores V, Emeruwa C, Shimonovich S, Roudnitsky V, Winer AG. Penile Preservation With Subcutaneous Transposition During Fournier’s Gangrene. Urol Case Rep. 2017 Apr 6;12:81-83. (License: CC BY-NC-ND-4.0)