Serous vs Mucinous Cystic Neoplasia – Location & Malignancy
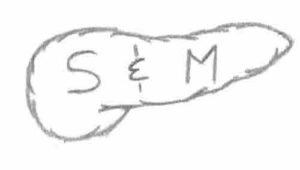
- Third Rule of Surgery: Don’t Mess With the Pancreas – “S&M” Written on the Pancreas
- Head (Serous) to Body/Tail (Mucinous)
- Benign (Serous/Side) to Malignant (Mucinous/Main/Mixed)
Mucinous Cystic Neoplasia Malignancy
- M-M: Mucinous – Malignant
Most Common Ages at Presentation of Pancreatic Cystic Neoplasia
- “Daughter-Mother-Grandma”
- Daughter – SPEN Most Common in Young Women (SP-Sprouts)
- Mother – MCN Most Common in Middle-Aged Women (M-Mother)
- Grandma – SCN Most Common in Older Women (S-Senile)