Endocrine: Parathyroidectomy
Minimally Invasive (Focused) Parathyroidectomy
Positioning
- Arms Tucked
- Neck Extended
Procedure
- Expose the Thyroid:
- Transverse “Kocher Incision”
- 1-2 Fingerbreadths Above Sternal Notch
- Traditional Incision: 8-10 cm Long – Generally Shorter (5-6 cm) in Modern Practice
- Minimally Invasive Incision: 2-4 cm Long
- Divide Platysma
- Superior Subplatysmal Flap Carried to Cricoid Cartilage
- Inferior Subplatysmal Flap Carried to Sternal Notch
- Divide Midline Raphe (Avascular Plane Between Strap Muscles)
- Dissect the Anterior Capsule of the Ipsilateral Thyroid Lobe from Medial to Lateral
- Transverse “Kocher Incision”
- Identify & Resect the Parathyroid Gland:
- Roll/Rotate the Ipsilateral Thyroid Medially
- Caution:
- Ensure Meticulous Intraoperative Hemostasis
- Avoid Thyroid Capsule Rupture
- Avoid Damage to Recurrent Laryngeal Nerve
- Avoid Damage to Normal Parathyroid Glands
- Identify & Resect the Diseased Parathyroid Gland
- Avoid Capsule Rupture – Causes Parathyromatosis (Diffuse Cervical Implantation)
- Avoid Injury to RLN & Inferior Thyroid Artery
- Verify Diseased Gland was Resected (Frozen Section vs Blood-Intact PTH)
- *See Below
- Finish & Close
- Obtain Hemostasis
- Close Strap Defect
- Close Platysma Defect
- Close Skin
“Miami Criteria” (Intraoperative PTH)
- Criteria: PTH Drop ≥ 50%
- Draws:
- Initial: Preoperative or Preexcision
- Comparison: 10- or 20-Minutes Post-Resection
- 97-99% Cure Rates
- If Fails to Drop 50%: Bilateral Exploration (Reasonable to Explore Ipsilateral First)
- If Drawn at 10-Minutes Do Not Need to Wait Until 20-Minutes
Confirmation of Gland Resection
- Frozen Section
- Confirm Parathyroid Tissue
- Ex-Vivo Aspiration of Gland
- Aspirate Intraoperative PTH > 1.5x Baseline Level
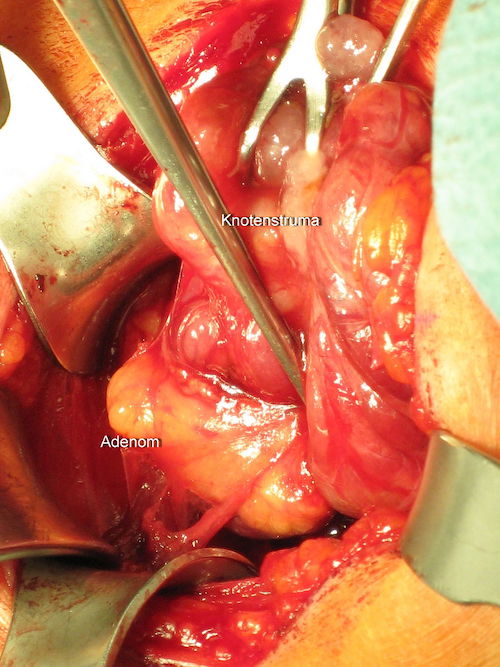
Parathyreoidectomy 1
Bilateral Neck Exploration
Positioning
- Arms Tucked
- Neck Extended
Procedure
- Expose the Thyroid:
- Transverse “Kocher Incision”
- 1-2 Fingerbreadths Above Sternal Notch
- Traditionally 8-10 cm Long – Generally Shorter (5-6 cm) in Modern Practice
- Divide Platysma
- Superior Subplatysmal Flap Carried to Cricoid Cartilage
- Inferior Subplatysmal Flap Carried to Sternal Notch
- Divide Midline Raphe (Avascular Plane Between Strap Muscles)
- Transverse “Kocher Incision”
- Expose Parathyroid Glands on One Side:
- Dissect the Anterior Capsule of One Lobe of the Thyroid from Medial to Lateral
- Roll/Rotate the Ipsilateral Thyroid Medially
- Identify the Ipsilateral Superior & Inferior Parathyroid Glands
- Caution:
- Ensure Meticulous Intraoperative Hemostasis
- Avoid Parathyroid Capsule Rupture – Causes Parathyromatosis (Diffuse Cervical Implantation)
- Avoid Thyroid Capsule Rupture
- Avoid Damage to Recurrent Laryngeal Nerve
- Expose Parathyroid Glands on the Contralateral Side
- Visually Inspect All Four Glands:
- 1-3 Glands Enlarged: Resect All Enlarged Glands
- 4 Glands Enlarged: Subtotal vs. Total Parathyroidectomy
- Finish & Close
- Obtain Hemostasis
- Close Strap Defect
- Close Platysma Defect
- Close Skin
Subtotal (3.5 Gland) Parathyroidectomy
- Resect 3.5 Glands, Leaving a Half Gland Behind
- First Resect the Half Gland, Then Resect the 3 Complete Glands
- Resect the Lateral Half of the Gland (Artery Enters Medially)
- Leave Equivalent Volume of a Normal Parathyroid Gland
Total Parathyroidectomy with Autoimplantation
- Resect All 4 Glands
- Harvest:
- Harvest an Equivalent Volume of a Normal Parathyroid Gland
- Use the Most Normal Appearing Gland
- Sharply Mince Tissue into a Fine Slurry
- Reimplantation:
- Expose Nondominant Brachioradilais Muscle in the Forearm
- Some Prefer to Use the Sternocleidomastoid Muscle in the Neck
- Make 3-4 Pockets in the Muscle Belly
- Place Equal Volumes of Slurry into Each Pocket
- Close Pockets with Nonabsorbable Suture
- Expose Nondominant Brachioradilais Muscle in the Forearm
Complications
Missing Gland
- Intraoperatively Unable to Find: Search
- Order of Search:
- Cervical Thymectomy (#1)
- Open Carotid Sheath (#2)
- Intraoperative Thyroid US
- May Consider Ipsilateral Thyroid Lobectomy if Needed
- Close if Still Unable to Find
- Order of Search:
- Postoperatively Still Unable to Find: Follow PTH
- Repeat Sestamibi Scan in 3-6 Months if PTH Still High
Hypocalcemia
- Causes:
- Transient Hypoparathyroidism
- Common After Parathyroidectomy from Suppressed Function
- Generally Regains Function After a Few Days
- Aparathyroidism
- Cause: Remnant/Graft Failure
- Labs: Decreased PTH, Normal Bicarb
- Hungry Bone Syndrome (HBS)
- Cause: High Calcium Absorption in Bone
- From Severe Pre-Operative Bone Disease
- Labs: Normal PTH, Decreased Bicarb
- Cause: High Calcium Absorption in Bone
- Transient Hypoparathyroidism
- Management: Monitor Ca/PTH Every 1-2 Weeks
- All Patient Should Empirically Be Given Oral Calcium Supplementation
- May Consider Oral Vitamin D Supplementation as Well
- Can Supplement Increased PO/IV Calcium as Needed
- All Patient Should Empirically Be Given Oral Calcium Supplementation
Hyperparathyroidism
- Persistent Hyperparathyroidism is Likely Due to a Missed Adenoma
- Recurrent Hyperparathyroidism is Likely Due to a New Adenoma or Tumor Implant
Cervical Hematoma
- Risk: 0.3-1.0%
- Must Ensure Meticulous Intraoperative Hemostasis
- Even Low-Volume Bleeding Can Cause Life-Threatening Airway Obstruction
- Can Cause Airway Edema from Venous/Lymphatic Obstruction Making Intubation Difficult
- Treatment:
- Respiratory Distress: Emergently Open at Bedside
- Not in Respiratory Distress: Intubate & Emergently Open in the OR
Recurrent Laryngeal Nerve Injury
- Risk: < 1%
- Prevention:
- Indications for Preoperative Laryngoscopy:
- Preoperative Hoarseness or Voice Changes
- History of Neck or Mediastinal Surgery
- Posterior Extrathyroidal Extension of Tumor
- Bulky Lymphadenopathy
- *Routine Assessment Unnecessary
- Intraoperative Nerve Monitoring (IONM):
- Surface Electrodes on the Endotracheal Tube Sense When the Recurrent Laryngeal Nerve is Stimulated
- Generally Recommended if There is a History of Prior Neck Surgery
- *Routine Use is Controversial
- Indications for Preoperative Laryngoscopy:
References
- Zimmerman T. Wikimedia Commons. (License: CC BY-3.0)