Pediatric Surgery: Abdominal Wall Pathology
Abdominal Wall Defects (Gastroschisis/Omphalocele)
Definitions
- Omphalocele
- Larger Defect (> 4 cm) at the Umbilicus
- Covered by Amniotic Membrane/Peritoneal Sac Mn
- Covered Bowel is Normal in Appearance
- Gastroschisis
- Smaller Defect (< 4 cm), Generally to the Right of the Umbilicus
- Not Covered by Amniotic Membrane/Peritoneal Sac
- Uncovered Bowel is Generally Normal at Birth but After 10-20 Minutes will Become Thickened, Matted & Edematous with Fibrous Peel from Amniotic Fluid/Meconium Staining
- Considered a Surgical Emergency (Bowel Not Covered)
- Most Common Abdominal Wall Defect
Proposed Pathogenesis
- Not Entirely Understood
- Omphalocele:
- Failure of Lateral Folds to Close
- Failure of Normal Counterclockwise Rotation Back into Abdomen
- Gastroschisis:
- Failure of Umbilical Coelom to Develop
- Yolk Sac & Vitelline Structures Fail to Incorporate into the Umbilical Cord
- Intrauterine Umbilical Vein Involution/Rupture
Associations
- All Have Intestinal Malrotation by Definition
- Omphalocele:
- Congenital Anomalies & Midline Defects are More Common
- Worse Overall Prognosis
- Cardiac Abnormalities (7-47%)
- Down Syndrome
- Cantrell Pentalogy
- Omphalocele
- Cardiac Defects
- Pericardial Defects
- Cleft Sternum
- Diaphragmatic Hernia
- Congenital Anomalies & Midline Defects are More Common
- Gastroschisis:
- Fewer Congenital Anomalies Than Omphalocele
- Intestinal Atresia More Common
Prenatal Period
- Most are Found on Prenatal US
- Cesarean Delivery is Not Necessary & Route of Delivery Does Not Affect Outcomes for Isolated Defects
Treatment
- Initial Management: Saline-Soaked Gauze Over the Bowel & Resuscitation
- Gauze Preserves Body Heat, Minimizes Insensible Fluid Loss & Protects Bowel
- Place NG/OG Tube for Decompression
- Open Abdominal Wall Defect if Too Tight & Causing Ischemia
- When Stable: Surgical Repair
- May Need Silastic Mesh Silo & Delayed Primary Repair if Too Tight
- Monitor for Abdominal Compartment Syndrome Postoperatively

Omphalocele
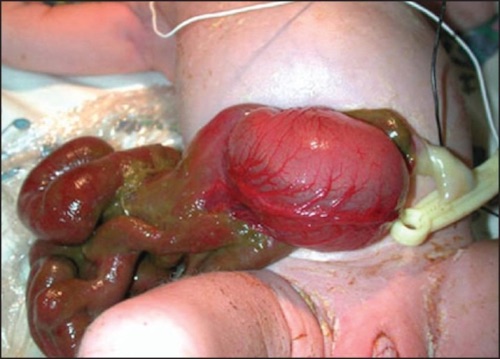
Gastroschisis 1

Gastroschisis Silo 2
Umbilical Defects
Umbilical Hernia
Umbilical Cord Hernia
- Smaller Defect (< 4 cm) at the Umbilicus
- Covered by Amniotic Membrane/Peritoneal Sac – Often Confused for Omphalocele
- Not Covered by Skin (Compared to Umbilical Hernia)
- Only Contains Midgut, Never Liver
- All Have Malrotation – Although Do Not Typically Cause Obstruction
- Abdominal Wall Superior to Defect is Normal – Rectus Meets in the Midline at Xiphoid
- Treatment: Reduction & Primary Fascial Closure
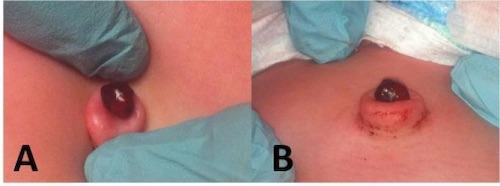
Patent Omphalomesenteric (Vitelline) Duct
- Presentation:
- Painless Chronic Mucus Drainage
- May See Feculent Drainage if the Entire Tract is Patent
- Small Bowel Obstruction
- US Shows a Tubular Structure
- Treatment: Surgical Resection
Omphalitis
- Definition: Infection of the Umbilicus & Surrounding Tissues
- Predominately Occurs in the Neonatal Period
- Most Common in Developing Countries
- High Mortality: 7-15%
- Presentation:
- Start Around 2-3 Days After Birth
- Umbilical/Periumbilical Pain
- Umbilical/Periumbilical Erythema & Induration
- Purulent Drainage from the Umbilical Stump
- Fever
- Risk Factors:
- Intentional Umbilical Nonseverance (“Lotus Birth”) – Umbilical Cord Not Separated After Birth
- Low Birth Weight
- Prolonged Labor
- Prolonged Rupture of Membranes
- Nonsterile Delivery
- Maternal Infection
- Cultural Application of Cow Feces
- Leukocyte Adhesion Disorders
- Diagnosis: Clinical
- Treatment: Broad Spectrum IV Antibiotics
- Generally Treated for 10 Day Course
Umbilical Granuloma
- Presentation: Painless Moist Pink-Red Lump of Tissue Seen After Umbilical Cord Has Separated
- Treatment: Silver Nitrate (Typically Requires Multiple Applications Over Several Weeks)
- If Fails: Ligation

Umbilical Cord Hernia Containing a Meckel’s Diverticulum 3

Patent Omphalomesenteric Duct, (A) Prolapsed Patent Duct, (B) Meconium Drainage from Patent Duct 4

Omphalitis 5
Umbilical Granuloma 6
Mnemonics
Omphalocele vs Gastroschisis
- Peritoneal Sac Covering:
- “O” – A Completed Ring Around a Peritoneal Sac
- “G” – Not a Complete Ring – Not Covered by a Peritoneal Sac
- Location:
- “O” at the Belly Button
References
- Wright NJ, Zani A, Ade-Ajayi N. Epidemiology, management and outcome of gastroschisis in Sub-Saharan Africa: Results of an international survey. Afr J Paediatr Surg. 2015 Jan-Mar;12(1):1-6. (License: CC BY-NC-SA-3.0)
- Dikshit VK, Gupta RK, Gupta AR, Kothari PR, Kamble RS, Kekre GA, Patil PS. Use of composite mesh in gastroschisis: A unique approach. Afr J Paediatr Surg. 2015 Apr-Jun;12(2):148-51. (License: CC BY-NC-SA-3.0)
- Gys B, Demaeght D, Hubens G, Ruppert M, Vaneerdeweg W. Herniation of a Meckel’s diverticulum in the Umbilical Cord. J Neonatal Surg. 2014 Oct 20;3(4):52. (License: CC BY-3.0)
- Kadian YS, Verma A, Rattan KN, Kajal P. Vitellointestinal Duct Anomalies in Infancy. J Neonatal Surg. 2016 Jul 3;5(3):30. (License: CC BY-3.0)
- Stagiryta. Wikimedia Commons. (License: CC BY-SA-4.0)
- Alexander G, Walsh R, Nielsen A. Neonatal umbilical mass. West J Emerg Med. 2013 Mar;14(2):163. (License: CC BY-NC-4.0)