Pediatric Surgery: Intraabdominal Malignancy
Neuroblastoma
Basics
- Origin: Neural Crest Cells
- Sites:
- Adrenal Medulla (50% – Most Common)
- Paraspinal Sympathetic Ganglion Chain (25%)
- Posterior Mediastinum (20%)
- Neck
- Pelvic Organ of Zuckerkandl
- Most Common Intraabdominal Malignancy in Peds Overall & < 2 Years
- Most Commonly Diagnosed Before Age 2
Prognosis
- Best Prognosis if Diagnosed Before 12-18 Months of Age
- May Have Spontaneous Regression
- Historically was 12 Months Prior to Recent Reviews
- Indicators of Poor Prognosis:
- Age > 18 Months
- N-myc Amplification with > 3-10 Copies
- DNA Ploidy
- Undifferentiated Histology
- MKI (Mitosis-Karyorrhexis Index) > 2-4%
- Distant Mets (Stage IV/M)
- Stage IV-S/MS is an Exception with Overall Survival > 90%
- Metastases are Common (Compared to Nephroblastoma)
Presentation
- Abdominal Mass (50-75%)
- Hypertension (25%)
- Abdominal Pain
- Intractable Diarrhea
- Malnutrition & Weight Loss
- Anemia
- “Panda Eyes” or “Racoon Eyes” (Periorbital Ecchymosis from Orbital Mets)
- “Blueberry Muffin” Lesions (Skin Mets)
- “Dancing Eye Syndrome” (Opsomyoclonus Myoclonus Syndrome) – Cerebellar Ataxia with Opsomyoclonus & Nystagmus
Staging
- International Neuroblastoma Staging System (INSS) – Old System
- I: Localized with Complete Excision & Negative Bilateral LN
- IIA: Localized with Incomplete Excision, Negative Bilateral LN
- IIB: Localized with Positive Ipsilateral LN, Negative Contralateral LN
- III: Tumor Crosses Midline or Localized Tumor with Positive Contralateral LN
- IV: Distant Mets
- IV-S: Localized Tumor (Defined for Stage I/II) in Children ≤ 1 Year with Mets Confined to Skin, Liver or Bone Marrow
- International Neuroblastoma Risk Group (INRG) Staging System – New System
- L1: Localized without Any Image-Defined Risk Factors (IDRF)
- L2: Locoregional with Presence of ≥ One Image-Defined Risk Factor (IDRF)
- M: Distant Mets (Except Stage MS)
- MS: Distant Mets in Children ≤ 18 Months with Mets Confined to Skin, Liver or Bone Marrow
- Children’s Oncology Group (COG) Risk Categorization
- Determines Low, Intermediate & High-Risk
- Based On:
- Stage
- Age
- N-myc Amplification
- DNA Ploidy
- International Neuroblastoma Pathology Classification (INPC)
Diagnosis
- Initial Imaging: CT/MRI
- Inferolateral Displacement of Kidney & Ureter
- Stippled Calcification of Tumor
- Staging: Metaiodobenzylguanidine (MIBG) Scan
- The Most Sensitive & Specific Modality for Staging Purposes
- Evaluates Both Soft Tissue & Bony Disease
- Definitive Diagnosis: Tissue Biopsy
- Incisional Biopsy of Tumor or Bone Marrow Aspirate/Biopsy of Metastases
- Histology: Small Round Blue Cells & Homer-Wright Pseudorosettes
- Evaluate Serum/Urine Catecholamine Levels
Treatment
- *Based on Children’s Oncology Group (COG) Risk Categorization
- Low-Risk: Surgical Excision
- May Require Ipsilateral Nephrectomy if Unable to Separate
- Intermediate-Risk: Neoadjuvant Chemotherapy & Surgical Excision
- High-Risk: Aggressive Multimodal Approach
- Neoadjuvant & Adjuvant Chemotherapy
- Surgical Excision (If Possible)
- Hematopoietic Stem Cell Transplantation
- Radiotherapy
- Biologic Immunotherapy
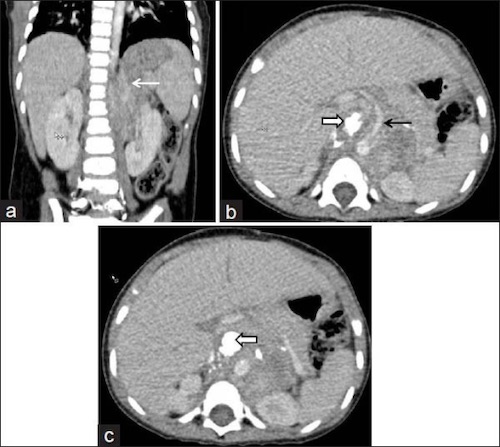
Neuroblastoma on CT – Crossing Midline & Encasing Aorta 1
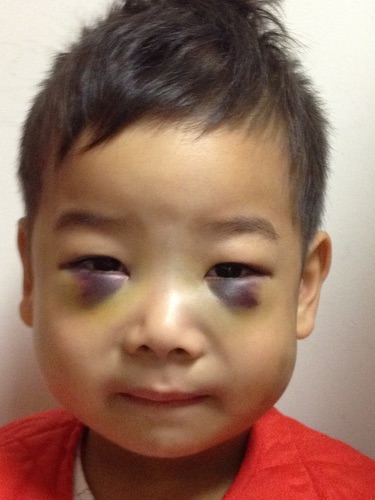
“Panda Eyes”/”Racoon Eyes” 2

Blueberry Muffin Syndrome 3
Nephroblastoma (Wilms Tumor)
Basics
- Second Most Common Intraabdominal Malignancy in Peds Overall
- Most Common Intraabdominal Malignancy in Peds > 2 Years
- Most Common (91%) Renal Tumor in Peds
- Most Commonly Diagnosed Between Ages 1-4
- Metastases are Uncommon (Compared to Neuroblastoma)
- Most Common Mets: Lung (10-20%)
- 5-Year Survival > 90%
Associations
- WAGR Syndrome
- Chromosome Defect in 11p13
- Includes:
- Wilms Tumor
- Aniridia (No Iris)
- Genitourinary Anomaly
- Mental Retardation
- 30-60% Risk for Wilms Tumor
- Denys-Drash Syndrome (DDS)
- Chromosome Defect in 11p13
- Includes:
- Renal Disease Since Birth Causes Early-Onset Renal Failure
- Ambiguous Genitalia
- 74% Risk for Wilms Tumor
- Beckwith-Wiedemann Syndrome
- Chromosome Defect in 11p15.5
- Includes:
- Macrosomia (Large Birth Size)
- Macroglossia (Large Tongue)
- Hemihypertrophy
- Visceromegaly
- Omphalocele
- Embryonal Tumors (Neuroblastoma, Nephroblastoma, Hepatoblastoma)
- 7-14% Risk for Wilms Tumor
Presentation
- Asymptomatic Abdominal Mass – Most Common Presentation
- Hematuria (18-24%)
- Hypertension (20-25%) – RASS Activation
- Coagulopathy (10%)
- Malnutrition & Weight Loss
- Left Varicocele – Tumor Obstruction of Spermatic Vein
Staging
- Children’s Oncology Group (COG) Staging System
- I: Localized with Complete Excision, No Rupture or Biopsy Prior to Removal, No Penetration of Renal Capsule or Involvement of Renal Sinus Vessels
- II: Extends Beyond Kidney Capsule but with Complete Excision, there is Penetration of Renal Capsule or Involvement of Renal Sinus Vessels
- III: Postoperative Residual Tumor or Tumor Ruptured/Biopsied Prior to Removal
- IV: Hematogenous or LN Mets Outside of the Abdomen
- V: Bilateral Renal Involvement
- Societe Internationale d-Oncologie Pediatrique (SIOP) Staging System
- I: The Tumor is Limited to the Kidney or Surrounded with a Fibrous Pseudocapsule, if Outside the Normal Contours of the Kidney. The Renal Capsule or Pseudocapsule May be Infiltrated with the Tumor, but it Does Not Reach the Outer Surface, and it is Completely Resected. The Tumor May be Protruding (Bulging) into the Pelvic System and Dipping into the Ureter, but it is Not Infiltrating the Walls. The Vessels of the Renal Sinus are Not Involved. Intrarenal Vessels May be Involved.
- II: The Tumor Extends Beyond the Kidney or Penetrates Through the Renal Capsule and/or Fibrous Pseudocapsule into the Perirenal Fat, but it is Completely Resected. The Tumor Infiltrates the Renal Sinus and/or Invades Blood and Lymphatic Vessels Outside the Renal Parenchyma, but it is Completely Resected. The Tumor Infiltrates Adjacent Organs or Vena Cava, but it is Completely Resected. The Tumor Has Been Surgically Biopsied (Wedge Biopsy) Prior to Preoperative Chemotherapy or Surgery.
- III: There is Incomplete Excision of the Tumor, Which Extends Beyond Resection Margins (Gross or Microscopic Tumor Remains Postoperatively). Any Positive Lymph Nodes are Involved. Tumor Ruptures Before or During Surgery (Irrespective of Other Criteria for Staging). The Tumor Has Penetrated the Peritoneal Surface. Tumor Implants are Found on the Peritoneal Surface. The Tumor Thrombi Present at Resection, Margins of Vessels or Ureter are Transected or Removed Piecemeal by Surgeon.
- IV: Hematogenous or LN Mets Outside of the Abdomen
- V: Bilateral Renal Involvement
Diagnosis
- Initial Imaging: CT/MRI
- Replacement of Renal Parenchyma
- Include Imaging of the Chest to Evaluate for Liver/Lung Mets
- Definitive Diagnosis: Histology (Surgical Excision or Tissue Biopsy)
- Classic Nephroblastoma Consists of 3 Cell Types:
- Blastemal Cells
- Stromal Cells
- Epithelial Cells (Glomeruli & Tubules)
- Role of Preoperative Tissue Biopsy Remains Controversial (Automatically Advanced to COG Stage III)
- Classic Nephroblastoma Consists of 3 Cell Types:
- Screen with US for High-Risk Genetic Syndromes
Treatment
- *Based on Either COG or SIOP Staging/Approaches (Differ Primarily Based on Timing of Chemotherapy)
- Primary Treatment: Nephrectomy & Chemotherapy
- Chemotherapy Regimens:
- COG Regimen – Adjuvant Treatment Only
- May Consider Nephrectomy Alone if Very-Low-Risk (Stage I with Favorable Histology & < 550g)
- SIOP Regimen – Neoadjuvant & Adjuvant Treatment
- May Consider Preoperative Chemotherapy Alone if Low-Risk Stage I
- COG Regimen – Adjuvant Treatment Only
- Add Adjuvant Radiation Therapy if Stage III/IV
- If Stage V (Bilateral): Attempt Nephron-Sparing Surgery
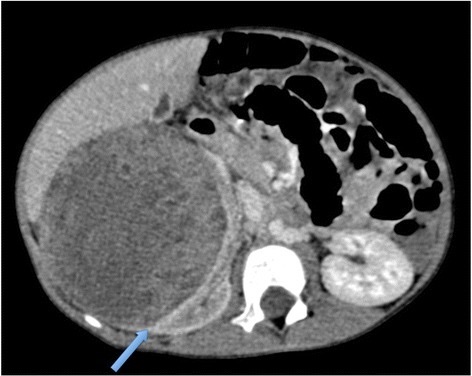
Nephroblastoma on CT with a “Claw Sign” (Blue Arrow) Showing Normal Renal Tissue Around the Tumor 4
Hepatoblastoma
Basics
- Most Common Primary Liver Tumor in Peds
- 50% of All Liver Masses in Peds
- 80% of All Malignant Liver Tumors in Peds
- More Than Half Are Unresectable or Have Distant Mets
Risk Factors & Associations
- Prematurity
- Very-Low-Birth-Weight
- Fetal Alcohol Syndrome
- Beckwith-Wiedemann Syndrome
- Hemihyperplasia/Hemihypertrophy
- Li-Fraumeni Syndrome
- Familial Adenomatous Polyposis (FAP)
Prognosis
- Best Prognosis: Fetal Histology
- Predictors of Poor Prognosis:
- Small Cell Undifferentiated (SCU) Histology
- Variants with Normal/Low AFP
- Older Age (≥ 8 Years at Diagnosis)
- Metastases
Presentation
- Asymptomatic Abdominal Mass – Most Common Presentation
- Moves with Respiration
- Abdominal Pain
- Abdominal Distention
- Bowel Obstruction from External Compression on Duodenum/Stomach
- Malnutrition
- Fatigue
Staging
- Children’s Oncology Group (COG) Staging System
- I: Complete Gross Resection at Diagnosis with Clear Margins
- II: Complete Gross Resection at Diagnosis with Microscopic Residual Disease at the Margins of Resection
- III: Biopsy Only at Diagnosis or Gross Total Resection with Nodal Involvement or Tumor Spill or Incomplete Resection with Gross Intrahepatic Disease
- IV: Metastatic Disease at Diagnosis
- PRETEXT: Pretreatment Extent (Of Tumor at Diagnosis)
- POSTTEXT: Posttreatment Extent (Of Tumor After Neoadjuvant Chemotherapy Before Surgery)
- PRETEXT/POSTTEXT Annotations:
- V – Involvement of the Vena Cava or All 3 Hepatic Veins
- P – Involvement of the Portal Bifurcation or Both Right and Left Branches
- E – Extrahepatic Contiguous Tumor Extension (Diaphragm or Stomach)
- C – Involvement of Caudate Lobe
- F – Multifocal Tumor
- R – Tumor Rupture at Diagnosis
Risk Stratification
- Children’s Oncology Group (COG) Risk Stratification
- Very Low Risk: Pure Fetal Histology Resected at Diagnosis (Stage I/II)
- Low Risk: Any Histology Resected at Diagnosis (Stage I/II)
- Intermediate Risk: Stage III, Including Small Cell Undifferentiated (SCU) Histology
- High Risk: Stage IV or AFP < 100 at Diagnosis
- Societe Internationale d-Oncologie Pediatrique – Epithelial Liver Tumor Study Group (SIOPEL) Risk Stratification
- Standard Risk:
- PRETEXT I-III
- High Risk:
- PRETEXT IV
- Metastasis at Diagnosis
- Small Cell Undifferentiated (SCU) Histology
- AFP < 100 at Diagnosis
- Standard Risk:
Diagnosis
- Initial Imaging: CT/MRI
- Include Chest & Brain to Evaluate for Mets
- Definitive Diagnosis: Tissue Biopsy
- Generally Required Although May Consider Skipping if Young (6 Months-3 Years) with Very High AFP Levels
- High AFP – Most Important Clinical Marker
Treatment
- Primary Treatment: Surgical Resection & Chemotherapy
- Chemotherapy Guidelines:
- COG Guidelines:
- PRETEXT I/II: Adjuvant Only
- PRETEXT III/IV: Neoadjuvant & Adjuvant
- SIOPEL Guidelines: Both Neoadjuvant & Adjuvant for All
- COG Guidelines:
- If Unresectable: Liver Transplant & Chemotherapy (Neoadjuvant & Adjuvant)
- Unresectable Indications: Stage III (With +V/P) or Stage IV
- Positive Margin: Adjuvant Chemotherapy & Monitor Imaging/AFP Levels
- Good Response Seen to Chemotherapy & Repeat Resection is Not Mandatory
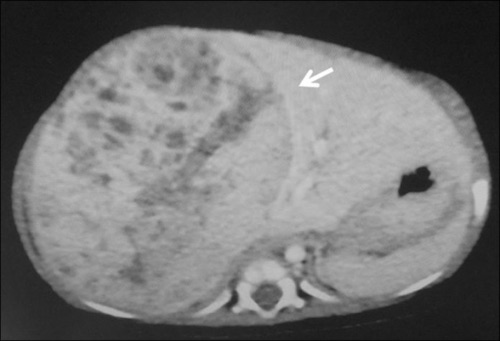
Hepatoblastoma on CT 5
References
- Dhamija E, Panda A, Das CJ, Gupta AK. Adrenal imaging (Part 2): Medullary and secondary adrenal lesions. Indian J Endocrinol Metab. 2015 Jan-Feb;19(1):16-24. (License: CC BY-NC-SA-3.0)
- Cheng, F.W.T., Ho, A.C.H. and Li, C.K. (2013), Raccoon eyes as presentation of lymphoblastic lymphoma in a child. Br J Haematol, 162: 2-2. (License: CC BY-4.0)
- Benmiloud S, Elhaddou G, Belghiti ZA, Hida M, Bouharrou A. Blueberry muffin syndrome [Blueberry muffin syndrome]. Pan Afr Med J. 2012;13:23. (License: CC BY-2.0)
- Dumba M, Jawad N, McHugh K. Neuroblastoma and nephroblastoma: a radiological review. Cancer Imaging. 2015 Apr 8;15(1):5. (License: CC BY-4.0)
- Kobayashi M, Mizuno M, Hasegawa Y, Nitta H, Wakabayashi G. Major liver resection by a hanging maneuver for an infant with hepatoblastoma. Am J Case Rep. 2012;13:140-2. (License: CC BY-NC-ND-3.0)