Stomach: Peptic Ulcer Disease (PUD)
Peptic Ulcer Disease (PUD)
Basics
- Definition: Macroscopic Mucosal Wounds Extending into the Submucosa or Muscularis Propria
- Sx: Dyspepsia (Epigastric Pain) that Improves with Eating
Risk Factors
- H. pylori (#1 Risk Factor)
- Helical GNR
- Resides in Mucous
- Pathophysiology:
- Starts in Antrum
- Induces Increased Gastrin (G Cells) & Acid (Parietal Cells) Secretion
- Causes Duodenal Ulcers
- With Continued Inflammation G Cells & Parietal Cells are Lost Causing Atrophy & Decreased Acid Secretion
- Causes Gastric Ulcers
- Bacteria Then Migrate Proximally with Corpus (Body) Gastritis
- Makes Urease: Splits Urea into Ammonia/Bicarbonate
- Alkaline Environment Promotes Survival
- Male
- Tobacco or Alcohol
- NSAIDs or Steroids
- Stress
Most Common Locations
- Within Stomach – Type I Along Lesser Curvature
- Within Duodenum – Anterior Aspect of First Portion
- Duodenum is the Most Common Site Overall
- 90% of Duodenal Ulcers are in the First Portion
- Distal Ulcers Raise Concern for Gastrinoma
Modified Johnson Classification for Gastric Ulcers
- Type I: Lesser Curvature, Low Along Body Mn
- Cause: Loss of Protection Mn
- Type II: Lesser Curvature & Duodenum
- Cause: Increased Acid
- Type III: Pre-Pyloric
- Cause: Increased Acid
- Type IV: Lesser Curvature, High Along Cardia Near GE Junction
- Cause: Loss of Protection
- Type V: Associated with NSAID’s
Special Ulcers
- Cushing Ulcer
- Ulcer from Head Trauma
- High ICP Causes Over-Stimulation of Vagus Nerve Which Causes Over-Secretion of Acid
- Curling Ulcer
- Ulcer from Burns
- Reduced Plasma Volume Causes Ischemia/Sloughing of Gastric Mucosa
- Cameron’s Ulcer
- Ulcer Within Hiatal Hernia
- Dieulafoy Ulcer (Dieulafoy’s Lesion/Calibre Persistent Artery)
- Vascular Malformation (Not PUD)
- *See Large Intestine: GI Bleed
- “Kissing” Duodenal Ulcer
- Ulcers of Both the Anterior & Posterior Duodenal Wall
- “Giant” Duodenal Ulcer (GDU)
- Ulcer ≥ 2 cm
- Usually Involves > 50% Circumference of the Duodenal Bulb
- NSAID Use More Common, H. pylori Less Common
- High Risk of Leak, Nonhealing & Stricture
Complications
- Bleeding
- Most Common Complication Overall
- Most Common Complication of Posterior Duodenal Ulcers (Affect GDA)
- Obstruction (Duodenum or Gastric Outlet)
- Perforation
- Most Common Complication in Stomach Ulcers
- Most Common Complication of Anterior Duodenal Ulcers
- Fistula
Testing
- Diagnosis:
- Stomach: EGD & Bx (Test for H. pylori & Rule Out Malignancy)
- Repeat After 2-3 Months
- Duodenum: EGD & Test for H. pylori
- Bx Not Routine Due to Higher Risk of Complications
- Bx Only if High Malignancy Risk, Obstructing or Giant (> 2 cm)
- Other Tests for H. pylori: Serology, Stool Antigen Test or Urea Breath Test
- Stomach: EGD & Bx (Test for H. pylori & Rule Out Malignancy)
- Detect H. pylori Eradication: Urea Breath Test
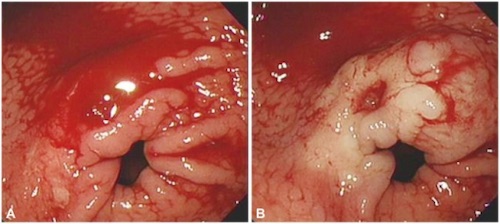
Bleeding Gastric Ulcer 1
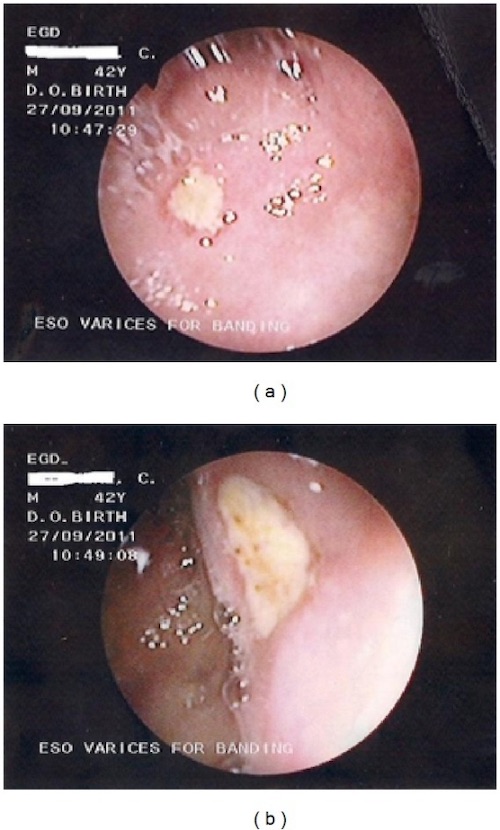
“Kissing” Duodenal Ulcer; (a) Anterior, (b) Posterior 2
Peptic Ulcer Disease (PUD) – Treatment
Primary Treatment
- H. pylori Negative: PPI
- H. pylori Positive: Triple/Quadruple Therapy
Refractory/Intractable (> 3 mo)
- Distal Stomach (Type I-III): Antrectomy
- If Type II/III: Add Truncal Vagotomy
- Caused by Increased Acid Production
- Reconstruction:
- Preferred: Billroth I
- Less Complications Than Billroth II
- If Inadequate Reach/Mobility of Duodenum: Billroth II or Roux-en-Y
- Preferred: Billroth I
- If Type II/III: Add Truncal Vagotomy
- Proximal Stomach (Type IV):
- ≤ 2 cm From Cardia: Csendes Procedure
- Distal Gastrectomy with In-Continuity Excision of Ulcer
- Reconstruction: Roux-en-Y
- May Consider Kelling-Madlener Procedure (Gastrectomy without Ulcer Excision)
- ≥ 5 cm Below Cardia: Pauchet Procedure
- More Limited Distal Gastrectomy
- Reconstruction: Billroth II or Roux-en-Y
- ≤ 2 cm From Cardia: Csendes Procedure
- Type V Stomach: Wedge Resection
- Duodenum: Truncal Vagotomy & Pyloroplasty
- Selective Has Too High Recurrence
Bleeding
- Initial: EGD
- Increased Risk of Rebleeding After EGD:
- Active Pulsatile Bleeding (Highest Risk – 80%)
- Visible Vessel (50%)
- Adherent Clot (15-25%)
- Clean Ulcer Base (< 5%)
- Increased Risk of Rebleeding After EGD:
- If Fails & Stable: Second EGD
- If Second Fails or Unstable: Surgery or Angioembolization
- Stomach – Gastrotomy & Oversew Vessel
- May Consider Wedge Resection if Along Greater Curvature
- Duodenum – Duodenotomy & Oversew Vessel
- Consider GDA Suture Ligation – Decreases Rate of Rebleeding
- Classic Technique: Triple Ligation
- One Above, One Below & One U-Stitch at the Left Aspect to Control Small Transverse Pancreatic Branches
- If Stable with Known Ulcer Diathesis: Add Truncal Vagotomy & Pyloroplasty
- Stomach – Gastrotomy & Oversew Vessel
Gastric Outlet Obstruction
- Initial Tx: Conservative Management (Bowel Rest, PPI & H. pylori Treatment)
- If Fails: Endoscopic Serial Dilations
- If Endoscopy Fails: Antrectomy & Vagotomy
- May Consider Vagotomy & Gastrojejunostomy Diversion Instead
Perforation
- May Consider Conservative Management (NGT, ABX & PPI) if Presentation Delayed (> 24 Hours), Contained & No Peritonitis
- Stomach:
- Stable: Same as Refractory Tx
- Unstable: Biopsy & Graham Patch or Wedge Resection
- Duodenum:
- Small (Most < 1 cm): Graham Patch
- Pyloric Exclusion with Gastrojejunostomy Indications:
- High Risk for Leak
- Too Large
- Poorly Controlled DM
- If Known Ulcer Diathesis: Add Highly Selective Vagotomy
- Contraindicated if > 24 Hours, Unstable or Extensive Peritonitis
- Pyloric Exclusion with Gastrojejunostomy Indications:
- “Giant” (≥ 2 cm):
- No Consensus on Specific Repair
- Options:
- Roux-en-Y with Roux Limb to Ulcer Edge
- Requires Kocher Maneuver & Debridement of Ulcer Edge
- Serosal Patch with Jejunal Loop
- Antrectomy & Billroth II Reconstruction
- Primary Repair & Triple-Tube-Ostomy
- Gastrostomy, Retrograde Duodenostomy & Feeding Jejunostomy
- Requires Kocher Maneuver to Minimize Tension & Debridement of Ulcer Edge
- Tube Duodenostomy
- Preferred Procedure if Unstable
- Procedure:
- Debride Ulcer Edges
- Place Malecot Catheter Through Defect
- Purse-String Suture Around Catheter
- Mobilize an Omental Pedicle
- Wrap Omental Pedicle Around the Tube & Secure at the Base
- Bring Malecot Externally to Drain
- Roux-en-Y with Roux Limb to Ulcer Edge
- Small (Most < 1 cm): Graham Patch
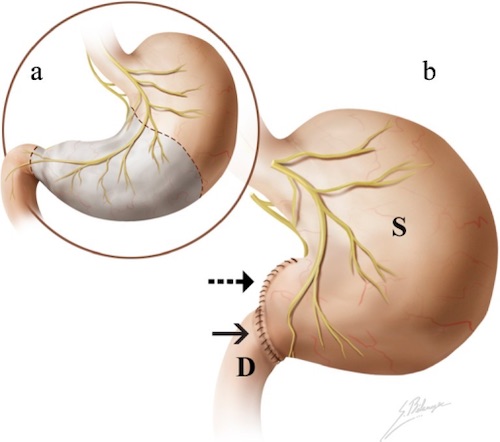
Antrectomy with Billroth I 3
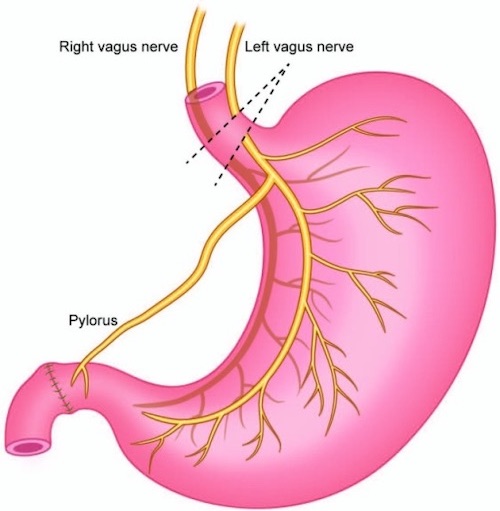
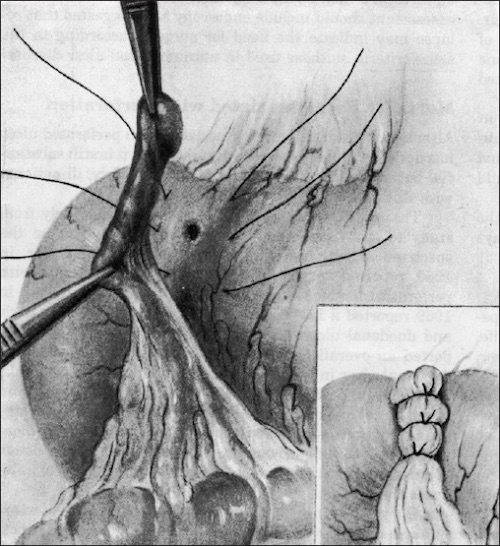
Truncal Vagotomy 4
Graham Patch 5
Mnemonics
Gastric Ulcer Sites
- 1 is Less/Low
- 2 Has Two
- 3 is Pre
- 4 at the Front Door
Gastric Ulcer Causes
- I/IV: Lesser Curvature, Loss of Protection
- II/III: Lower, Where Acid Lies
- V: Anywhere, NSAIDs
References
- Kim JS, Park SM, Kim BW. Endoscopic management of peptic ulcer bleeding. Clin Endosc. 2015 Mar;48(2):106-11. (License: CC BY-NC-3.0)
- Oluyemi A, Amole A. Portal hypertensive duodenopathy manifesting as “kissing” duodenal ulcers in a nigerian with alcoholic cirrhosis: a case report and brief review of the literature. Case Rep Med. 2012;2012:618729. (License: CC BY-3.0)
- Terrone DG, Lepanto L, Billiard JS, Olivié D, Murphy-Lavallée J, Vandenbroucke F, Tang A. A primer to common major gastrointestinal post-surgical anatomy on CT-a pictorial review. Insights Imaging. 2011 Dec;2(6):631-638. (License: CC BY-2.0)
- Rabben HL, Zhao CM, Hayakawa Y, Wang TC, Chen D. Vagotomy and Gastric Tumorigenesis. Curr Neuropharmacol. 2016;14(8):967-972.(License: CC BY-NC-4.0)
- Maghsoudi H, Ghaffari A. Generalized peritonitis requiring re-operation after leakage of omental patch repair of perforated peptic ulcer. Saudi J Gastroenterol. 2011 Mar-Apr;17(2):124-8. (License: CC BY-2.0)