Trauma: Peripheral Nerve Injury
Peripheral Nerve Injury
Types of Injury
- Neurapraxia
- Injury: Focal Demyelination
- No Damage to Axon or Connective Tissue
- Reversible
- Injury: Focal Demyelination
- Axonotmesis
- Injury: Axon Damaged
- Connective Tissue (Epineurium, Perineurium & Endoneurium) Preserved
- Reversible
- Injury: Axon Damaged
- Neurotmesis
- Injury: Total Transection of Axon & Connective Tissue
- Non-Reversible
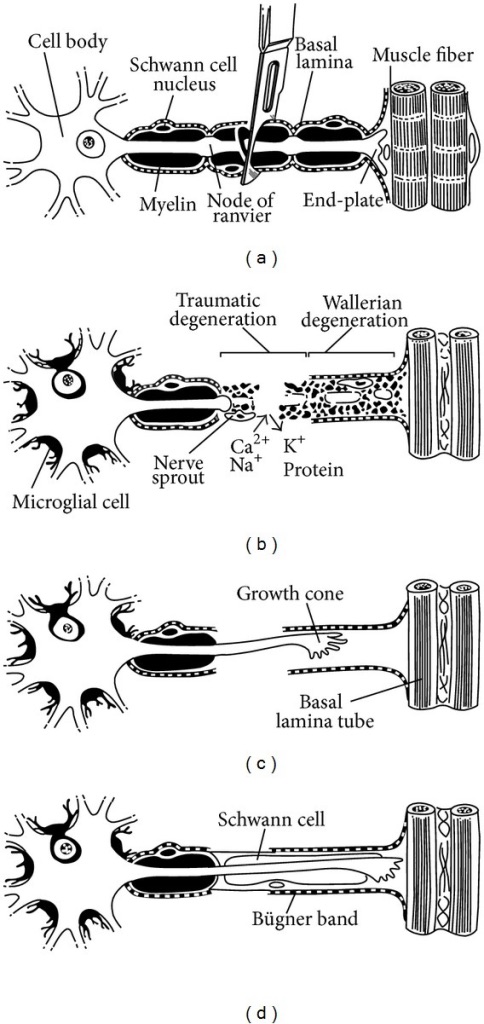
Regeneration
- Regeneration Rate: 1-2 mm/Day
- Wallerian Degeneration: Degeneration of Distal Axon to Create Microenvironment Conductive for Regeneration & Reinnervation
- Primarily Mediated by Schwann Cells
Brachial Plexus Injury (BPI)
- Law of 70’s:
- 70% Due to Traffic Accidents
- 70% of Those Involve Motorcycles or Bicycles
- 70% Sustain Multiple Injuries
- 70% Sustain a Lesion of the Supraclavicular Plexus
- 70% of These Have ≥ 1 Plexus Root Avulsion
- 70% Also Sustain Root Avulsions of the Lower Plexus
- 70% of Lower Root Avulsions Experience Chronic Pain
Burner Syndrome
- Also Known as a “Stinger” Injury
- Cause: Trauma to the Base of the Neck/Shoulder
- Most Common in Collision Sports (Football, Hockey, Wrestling)
- Pathophysiology: Stretching of the Spinal Roots
- Most Common in Upper Roots (C5/C6)
- Presentation:
- Sustained Paresthesia
- Burning Sensation Down the Lateral Arm
- Usually Transient – Sensory Function Returns Before Motor Function
- Lasts Minutes-Days
- Diagnosis: History & Physical Exam
- Consider Electromyography (EMG) if Symptoms Persist Longer than 3 Weeks
- Treatment: Observation
Treatment
- Closed Injury
- Neurapraxia: Conservative Management
- Axonotmesis vs Neurotmesis: Electrodiagnostic Studies After 3-6 Months
- Axonal Recovery (Axonotmesis): Conservative Management
- No Axonal Recovery: Surgery & Monitor for Action Potentials Across Lesion
- Action Potentials Recorded (Axonotmesis) – Conservative Treatment
- No Action Potentials Recorded (Neurotmesis) – Surgical Repair
- Open Injury
- Lesion in Continuity: Conservative Management
- Lesion in Discontinuity:
- Laceration: Immediate Repair
- Blunt Transection: Early Repair (2-4 Weeks)
- Allow Decreased Inflammation
- *May Require Radial/Sural Nerve Graft if Contracted
Peripheral Nerve Degeneration & Regeneration 1

Vascularized Sural Nerve Graft 1
References
- Grinsell D, Keating CP. Peripheral nerve reconstruction after injury: a review of clinical and experimental therapies. Biomed Res Int. 2014;2014:698256. (License: CC BY-3.0)