Cardiothoracic Surgery: Pneumonia (PNA)
Pneumonia (PNA) – Definitions
Definition
- Pneumonia (PNA): Acute Infection of Pulmonary Parenchyma
Types
- Community-Acquired Pneumonia (CAP): Acquired Outside of the Hospital
- Typical Pneumonia: Typical Organisms Cultured of Standard Media
- Atypical Pneumonia: Atypical Organisms Not Cultured on Standard Media
- Healthcare-Associated (Nosocomial) Pneumonia (HCAP): Acquired in the Hospital Setting
- Hospital-Acquired Pneumonia (HAP): Acquired ≥ 48 Hours After Hospital Admission
- *Differentiation Between HCAP, HAP & Nosocomial PNA Varies
- Ventilator-Associated Pneumonia (VAP): Acquired ≥ 48 Hours After Intubation
- Hospital-Acquired Pneumonia (HAP): Acquired ≥ 48 Hours After Hospital Admission
- Aspiration Pneumonia: Associated with Aspiration of Material into the Lower Respiratory Tract
Pneumonia (PNA) – Microbiology
Community-Acquired Pneumonia (CAP) Organisms
- Typical Organisms:
- Streptococcus pneumonia – Most Common Cause of CAP
- Klebsiella pneumonia
- Hemophilus influenzae
- Pseudomonas aeruginosa
- Staphylococcus aureus
- Atypical Organisms:
- Legionella
- Mycoplasma pneumonia
- Chlamydia pneumonia
Healthcare-Associated Pneumonia (HCAP) Organisms
- Staphylococcus aureus
- Methicillin-Sensitive Staphylococcus aureus (MSSA)
- Methicillin-Resistant Staphylococcus aureus (MRSA) – Most Common Cause of HCAP
- Pseudomonas aeruginosa
- Klebsiella pneumonia
- Escherichia coli
- Enterobacter spp
- Acinetobacter spp
- Streptococcus pneumonia
Common Contaminants
- Staphylococcus epidermidis
- Candida spp
- Streptococcus viridians
- Corynebacterium diphtheriae
HCAP Multidrug-Resistant (MDR) Risk Factors
- MDR Risk Factors:
- IV Antibiotic Use within the Last 90 Days
- VAP-Specific Risk Factors:
- Prolonged (≥ 5 Days) Hospitalization Prior to VAP Onset
- Septic Shock at Time of VAP Onset
- ARDS Prior to VAP Onset
- Acute Renal Replacement Therapy Prior to VAP Onset
- MRSA Risk Factors:
- Colonization with or Prior Isolation of MRSA
- ICU/Unit with > 10-20% of S. aureus Isolates Being Methicillin-Resistant
- ICU/Unit with Unknown MRSA Prevalence
- MDR Gram-Negative Bacilli (Pseudomonas or Other) Risk Factors:
- Colonization with or Prior Isolation of MDR Gram-Negative Bacilli (Pseudomonas or Other)
- HAP-Specific Risk Factors:
- Structural Lung Disease (Bronchiectasis or Cystic Fibrosis)
- Respiratory Specimen Gram Stain with Numerous Gram-Negative Bacilli
- VAP-Specific Risk Factors:
- ICU with > 10% of Gram-Negative Isolates Resistant to an Agent Considered for Monotherapy
- ICU with Unknown Local Antimicrobial Susceptibility Rates
- HAP Risk Factors for Increased Mortality:
- Requires Ventilator Support for HAP
- Septic Shock
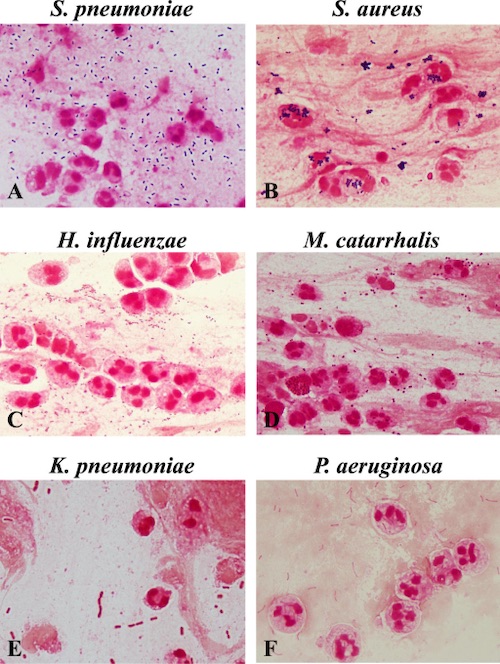
Pneumonia Gram Stains 1
Pneumonia (PNA) – Diagnosis
Presentation
- Fever
- Cough
- Pleuritic Chest Pain
- Purulent Sputum
- Tachypnea
- Dyspnea
- Hypoxia
- Ventilator Changes:
- Reduced Tidal Volume
- Increased Inspiratory Pressures
- Leukocytosis
Diagnosis
- Gold Standard: Lung Biopsy (Invasive & Rarely Used)
- Clinical Diagnosis: New Lung Infiltrate on Imaging with Clinical Evidence
- CXR Has Overall Low Sensitivity & Specificity
- Culture Supports Diagnosis & Guides Therapy
- Indicators of Good-Quality:
- Moderate-Many Polymorphonuclear Leukocytes
- Few-No Squamous Epithelial Cells
- VAP Thresholds:
- Endotracheal Aspirate > 1,000,000 (106) CFU/mL
- Bronchoalveolar Lavage (BAL) > 10,000 (104) CFU/mL
- Protected Specimen Brush (PSB) > 1,000 (103) CFU/mL
- *Should Be Obtained Prior to Initiation of Antibiotics
- Indicators of Good-Quality:
Culture Types
- Sputum Culture – Expectorated Sputum, Ideally from a Deep Cough
- Endotracheal Aspirate – Aspirated Sputum from a Catheter Passed into the Trachea, Possibly Through an Endotracheal Tube
- Bronchoalveolar Lavage (BAL) – Using a Bronchoscope the Distal Bronchi are Washed with Saline & Then Suctioned for Culture
- *See Endoscopy: Respiratory Endoscopy
- Obtains a Large Sample than PSB & Often Preferred
- Mini-BAL – Catheter Blindly Advanced Through an Endotracheal Tube Until Resistance is Met Followed by Infusion of Three 50 cc Aliquots of Saline & Aspiration
- Protected Specimen Brush (PSB) – Using a Bronchoscope the Distal Bronchi are Brushed for Culture
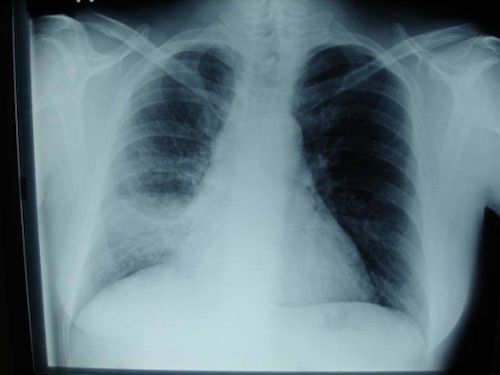
Pneumonia on CXR 2

Pneumonia on CT 3
Pneumonia (PNA) – Treatment
CAP Treatment Regimen
- Primary Treatment: Antibiotics
- *Antibiotic Regimen Varies Based on Risk Factors, Allergies & Unit of Admission
HCAP Treatment Regimen
- No MDR Risks: Single-Drug Therapy
- MRSA Risk: Two-Drug Therapy (Single-Drug Plus MRSA Coverage)
- MDR Gram-Negative Bacilli Risk: Two-Drug Therapy (Single-Drug Plus MDR Gram-Negative Bacilli Coverage)
- MDR Risk: Three-Drug Therapy (Single-Drug Plus MRSA Coverage & MDR Gram-Negative Bacilli Coverage)
- Other Indications for Three-Drug Therapy:
- HAP with Increased Mortality Risk
- Both MRSA & Gram-Negative Bacilli Risk
- Other Indications for Three-Drug Therapy:
HCAP Antibiotic Options
- Single-Drugs:
- Piperacillin-Tazobactam (Zosyn)
- Cefepime
- Levofloxacin
- Meropenem
- MRSA Coverage:
- Vancomycin
- Linezolid
- MDR Gram-Negative Bacilli Coverage:
- Aminoglycosides:
- Amikacin
- Gentamicin
- Tobramycin
- Fluoroquinolones:
- Levofloxacin
- Ciprofloxacin
- Aztreonam
- Aminoglycosides:
References
- Fukuyama H, Yamashiro S, Kinjo K, Tamaki H, Kishaba T. Validation of sputum Gram stain for treatment of community-acquired pneumonia and healthcare-associated pneumonia: a prospective observational study. BMC Infect Dis. 2014 Oct 18;14:534.(License: CC BY-4.0)
- Bartziokas K, Daenas C, Preau S, Zygoulis P, Triantaris A, Kerenidi T, Makris D, Gourgoulianis KI, Daniil Z. Vibration response imaging: evaluation of rater agreement in healthy subjects and subjects with pneumonia. BMC Med Imaging. 2010 Mar 11;10:6. (License: CC BY-2.0)
- Miyashita N, Sugiu T, Kawai Y, Oda K, Yamaguchi T, Ouchi K, Kobashi Y, Oka M. Radiographic features of Mycoplasma pneumoniae pneumonia: differential diagnosis and performance timing. BMC Med Imaging. 2009 Apr 29;9:7.(License: CC BY-2.0)