Anorectal: Proctectomy
Low Anterior Resection (LAR)
Basics
- Resection of Sigmoid & Rectum
- Spares Internal Anal Sphincter
- Requires Splenic Flexure Mobilization
Open Procedure
- Mobilize the Sigmoid & Left Colon
- Pack & Retract Small Bowel to the Right with a Moist Lap Pad
- Retract Sigmoid Medially
- Dissect Colon Lateral-to-Medial Along the White Line of Toldt
- Continue Dissection in This Plane Bringing the Left Colon Away from Gerota’s Fascia
- Care to Preserve Gonadal Vessels & Left Ureter
- Enter the Retrorectal Avascular Plane at the Base of the Sigmoid Mesocolon
- Identify & Ligate the Inferior Mesenteric Vessels
- Retract Sigmoid to the Right
- Identify & Divide IMA 1-2 cm From the Aortic Origin
- Identify &Divide IMV at the Ligament of Treitz – Allows Full Mobilization of the Splenic Flexure
- Mobilize Splenic Flexure
- Continue Lateral Dissection Superiorly
- Take Down Colonic Pancreatic Attachments
- Take Down Omental Attachments at the Distal Transverse Colon
- Divide the Sigmoid Colon
- Divide Sigmoid Mesentery to the Bowel Wall
- Staple Division of the Sigmoid Colon
- Sharply Dissect Circumferentially Around the Mesorectum
- Pack Left Colon Superiorly & Retract Sigmoid Anteriorly
- Start Dissection Posterior & Then Move Lateral
- Avoid Injury to the Superior & Inferior Hypogastric Plexuses
- Avoid Injury to the Lateral Hypogastric & Pelvic Parasympathetic Nerves
- Finish Dissection Anteriorly Along Denovilliers’ Fascia
- *Blunt Dissection Associated with Higher Recurrence – 25% Positive Resection Margin
- Divide the Rectum
- First Irrigate the Rectum from Below with Saline or Water – Possibly Decreases Recurrence by Exfoliated Malignant Cells Although Uncertain
- Transect Rectum with a Linear Stapler
- Remove Specimen
- Complete Coloanal Anastomosis
- Hand-Sewn or EEA Circular Stapler
- Air Leak Test to Confirm Integrity of Anastomosis
Variations
- Can Be Preformed Open, Laparoscopic or Robotic
- “Hybrid” Approach Using a Combination of Laparoscopy & An Open Lower Midline/Pfannenstiel Incision for Hand-Assist
- When Done Entirely Laparoscopic – Dissection Proceeds Medial-to-Lateral
- First Dissect Vessels, Then Takedown Splenic Flexure & Lateral Attachments
Ostomy Indications
- Diverting Loop Ileostomy
- Low < 5 cm from Anal Verge
- High-Risk for Leak
- Hartmann’s Procedure
- Distant Mets Noted – Will Require Chemotherapy (Leak Can Delay Tx & Higher Risk or Enteritis)
Complications
- Bleeding
- Urethral Injury
- LAR Syndrome
- Sx: Fecal Incontinence, Tenesmus & Fecal Urgency
- Causes:
- Colonic Dysmotility
- Decreased Rectal Sensibility
- Loss of Anorectal Reflex
- Anal Sphincter Dysfunction or Nerve Damage
- Affects 25-80% of Patients to Some Degree
- Most Improve Over 6-12 Months
- Tx: Fiber & Antimotility Agents
- If Fails: Sacral Nerve Stimulator
- Anastomotic Leak & Pelvic Sepsis
- Anastomotic Stricture
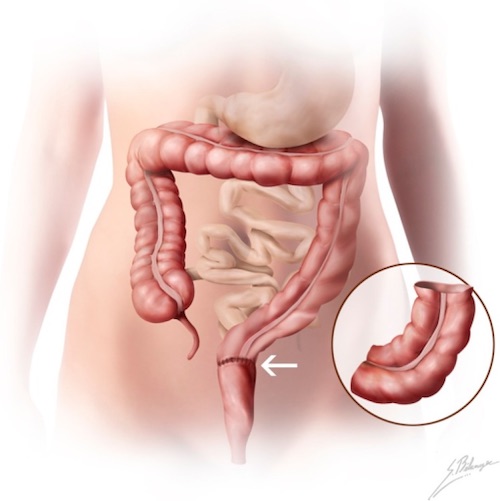
LAR 1
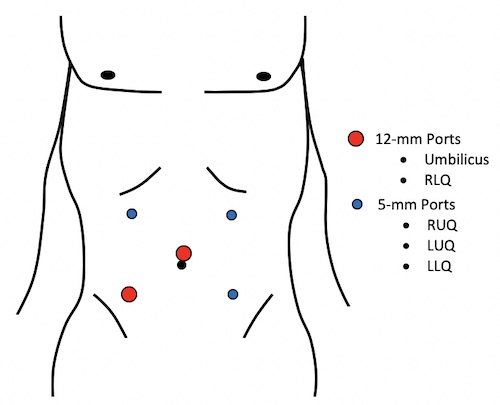
LAR Port Placement
Abdominoperineal Resection (APR)
Basics
- Resection of Sigmoid, Rectum & Anus
- Loss of Internal Anal Sphincter
- Requires a Permanent Colostomy
- Splenic Flexure Mobilization Not Required
Abdominal Dissection
- Mobilize the Sigmoid & Left Colon
- Pack & Retract Small Bowel to the Right with a Moist Lap Pad
- Retract Sigmoid Medially
- Dissect Sigmoid Lateral-to-Medial Along the White Line of Toldt
- Continue Dissection in This Plane Bringing the Left Colon Away from Gerota’s Fascia
- Care to Preserve Gonadal Vessels & Left Ureter
- Enter the Retrorectal Avascular Plane at the Base of the Sigmoid Mesocolon
- Identify & Ligate the Inferior Mesenteric Vessels
- Retract Sigmoid to the Right
- Identify & Divide IMA 1-2 cm From the Aortic Origin
- Identify & Divide IMV at the Ligament of Treitz – Allows Full Mobilization of the Splenic Flexure
- Sharply Dissect Circumferentially Around the Mesorectum
- Retract Sigmoid Anteriorly
- Start Dissection Posterior & Then Move Lateral
- Avoid Injury to the Superior & Inferior Hypogastric Plexuses
- Avoid Injury to the Lateral Hypogastric & Pelvic Parasympathetic Nerves
- Finish Dissection Anteriorly Along Denovilliers’ Fascia
- *Blunt Dissection Associated with Higher Recurrence
- Divide the Sigmoid Colon
- Divide Sigmoid Mesentery to the Bowel Wall
- Staple Division of the Sigmoid Colon
- Dissect as Far into Pelvis as Possible Including Wide Mesenteric Excision (WME)
- Create End Colostomy
- Typically Done After Perineal Dissection if in Lithotomy Position
- Can Be Done Before if Positioning Prone for Perineal Dissection
Perineal Dissection
- Approach:
- Traditional/Standard Resection – “Waist” Resection
- “Coned In” Sparing the Levators
- Extended/Extralevator (ELAPE) – “Cylinder” Resection
- “Cylindrical” with Wide Resection of Levators
- Preferred if Tumor Invades External Sphincter or Levators
- Some Argue Lower Rates of Positive Margins Although Literature Shows No Improved Outcomes
- Higher Rates of Wound Complications
- Traditional/Standard Resection – “Waist” Resection
- Close Anus with Purse-String Suture
- Wide Vertical Elliptical Incision Around the Anus
- Dissect into the Ischiorectal Space
- Start Posteriorly Over the Coccyx
- Divide the Anococcygeal Raphe
- Divide Waldeyer’s Fascia & Enter the Presacral Space
- Divide Superficial Fascia Laterally
- Continue Posterior Dissection While Elevating the Rectum
- Identify & Divide the Lateral Levator Muscles
- Insert Finger into Presacral Space & Sweep Laterally
- Divide Levator Muscles Bilaterally
- Finish Dissection Anteriorly
- Retract Rectum Inferiorly & Posteriorly
- Avoid Injury to Urethra or Vaginal Wall from Dissecting Too Anteriorly
- Once Able, The Sigmoid is Delivered Through the Posterior End & with Traction the Final Levator Attachments & Transected
- Start Posteriorly Over the Coccyx
- Remove Specimen Through the Pelvic Ring
- Close Perineum in Multiple Layers with Vertical Mattress on the Skin
- Consider Rotational Pedicle Flap if Received Neoadjuvant Radiation – Often Use Rectus Abdominis Muscle Flap (Large & Avoids Radiated Skin)
Complications
- Perineal Wound Complications
- Common (36-80%)
- Risk Factors: Prior XRT, Malnutrition, Smoking & Obesity
- Autonomic Nerve Injury
- Sympathetic Nerves
- Sx: Increased Bladder Tone, Reduced Capacity & Impaired Ejaculation
- Parasympathetic System
- Sx: Voiding Difficulty, Erectile Dysfunction & Decreased Vaginal Lubrication
- Sympathetic Nerves
- Bleeding/Hematoma (0-4%)
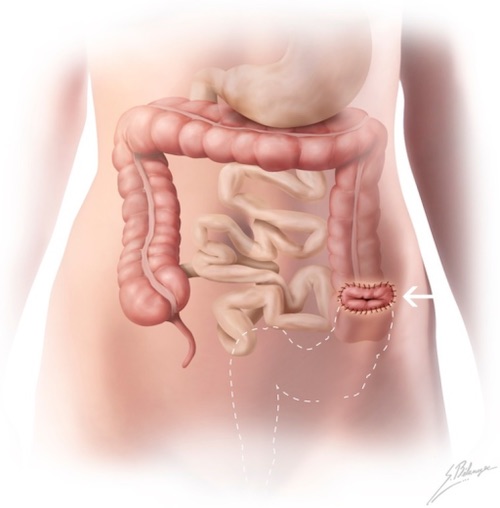
APR 1
References
- Terrone DG, Lepanto L, Billiard JS, Olivié D, Murphy-Lavallée J, Vandenbroucke F, Tang A. A primer to common major gastrointestinal post-surgical anatomy on CT-a pictorial review. Insights Imaging. 2011 Dec;2(6):631-638. (License: CC BY-2.0)