Urology: Prostate Cancer
Prostate Cancer
Types of Cancer
- Adenocarcinoma (> 95%)
- Neuroendocrine Tumor
- Urothelial (Transitional Cell) Carcinoma
- Basal Cell Carcinoma
- Lymphoma
Location
- Most Common Site: Posterior Lobe
- Most Common Site of Metastasis: Bone
- Osteoblastic Lesion with High Alk-Phos
- Lymphatic Spread
Presentation
- Usually Asymptomatic at Time of Diagnosis
- Nonspecific Lower Urinary Tract Symptoms (LUTS)
- Hematuria
Prostate Specific Antigen (PSA)
- Causes of Increased Level:
- Benign Prostatic Hyperplasia (BPH)
- Prostatitis
- Prostate Cancer
- Changes After Prostatectomy:
- Should Be Zero by Week 3
- If Not: Suspect Mets
Screening
- Normal Risk: PSA at Age 50-55
- High Risk: PSA After Age 40-45, Every 1-2 Years
- *No Role for Digital Rectal Exam (DRE) in Screening
Diagnosis
- Primary Diagnosis: Transrectal US-Guided Biopsy
- Can Also Use MRI to Guide Biopsy
- Generally Perform x12 Core Biopsies to Increase Detection Rate
- Gleason Grading System Used to Describe
Gleason Grading System
- Based Solely on Architecture of the Cancer Cells
- Higher Score Indicates Higher Risk of Metastatic Disease & Poor Outcomes
- Gleason Grade: For the Individual Cells
- Scored: 1-5 (Most-Least Differentiated)
- Gleason Score: For the Specimen
- Addition of the Grades for the Two Most Predominant Patterns
- Combined Scores: 2-10 (2-5 are Generally Not Diagnosed as Cancer)
- *The Preferred Grading System
- Gleason Grade Group:
- Provides Greater Risk Stratification
- Does Not Replace the Gleason Score but Should Be Given in Addition
- Group 1: Score ≤ 6
- Group 2: Score 7 (3+4) – Hazard Ration for Death 2.8 Relative to Group 1
- Group 3: Score 7 (4+3) – HR 6.0 Relative to Group 1
- Group 4: Score 8 – HR 7.1 Relative to Group 1
- Group 5: Score 9-10 – HR 12.7 Relative to Group 1
Prostate Cancer 1
TNM Staging
- TNM
| Clinical T (cT) | Pathologic T (pT) | N | M | |
| 1 | Not Palpable 1a – Incidental Finding in ≤ 5% of Tissue Resected 1b – Incidental Finding in > 5% of Tissue Resected 1c – Identified by Needle Biopsy | *None | Regional LN+ | Mets 1a – Nonregional LN 1b – Bones 1c – Other Sites |
| 2 | Palpable but Confined to Prostate 2a – Involves ≤ Half of One Side 2b – Involves > Half of One Side 2c – Involves Both Sides | Confined to Prostate | ||
| 3 | Extraprostatic Tumor but Not Fixed 3a – Extraprostatic Extension 3b – Invades Seminal Vesicles | Extraprostatic Tumor but Not Fixed 3a – Extraprostatic Extension 3b – Invades Seminal Vesicles | ||
| 4 | Fixed or Invades Adjacent Structures (Other than Seminal Vesicles) | Fixed or Invades Adjacent Structures (Other than Seminal Vesicles) |
- Staging
| T | N | M | PSA | G | ||
| I | cT1-2a, pT2 | N0 | M0 | < 10 | 1 | |
| II | A | cT1-2a, pT2 | N0 | M0 | 10-19 | 1 |
| cT2b-c | N0 | M0 | < 20 | 1 | ||
| B | T1-2 | N0 | M0 | < 20 | 2 | |
| C | T1-2 | N0 | M0 | < 20 | 3-4 | |
| III | A | T1-2 | N0 | M0 | ≥ 20 | 1-4 |
| B | T3-4 | N0 | M0 | Any | 1-4 | |
| C | Any T | N0 | M0 | Any | 5 | |
| IV | A | Any T | N1 | M0 | Any | Any |
| B | Any T | Any N | M1 | Any | Any | |
- *G = Group Grade
Management Options
- Radiation Therapy (RT)
- External Beam Radiation Therapy (EBRT)
- Brachytherapy
- Androgen Deprivation Therapy (ADT)
- Medical Castration: Leuprolide (GnRH Agonist)
- Prevent a Transient LH Surge with Flutamide (Antiandrogen)
- Surgical Castration: Bilateral Orchiectomy
- Medical Castration: Leuprolide (GnRH Agonist)
- Radical Prostatectomy
- Surgical Resection of the Prostate, Seminal Vesicles & Lymph Nodes
Treatment Approach
- Confined to Prostate: RT or Radical Prostatectomy
- *Consider Active Surveillance for Very Low-Low Risk Tumors
- *Consider Adding ADT for High-Risk Tumors
- Locally Advanced or Nodal Involvement: RT & ADT
- May Consider Radical Prostatectomy
- Metastatic Disease: ADT
- Also Consider Docetaxel in Metastatic Disease
References
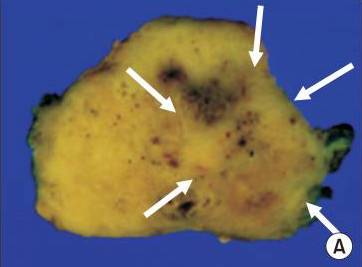
- Yoo S, Kim JK, Jeong IG. Multiparametric magnetic resonance imaging for prostate cancer: A review and update for urologists. Korean J Urol. 2015 Jul;56(7):487-97. (License: CC BY-NC-3.0)