Vascular: Pulmonary Embolism (PE)
Pulmonary Embolism (PE)
Basics
- Most Common Source: Iliofemoral DVT
- Risk for Sudden Cardiac Arrest & Circulatory Collapse
- 30% Mortality if Untreated
Physiology
- Mechanisms of Impaired Gas Exchange:
- Mechanical/Functional Obstruction (Ventilation-Perfusion Mismatch)
- Inflammation Causing Surfactant Dysfunction & Atelectasis (Functional Intrapulmonary Shunting)
- Impaired Gas Exchange Causes to Hypoxia
- Hypoxia Causes Tachycardia & Tachypnea
- Tachypnea Leads to Hypocapnia & Respiratory Alkalosis
Presentation
- Many are Asymptomatic
- Dyspnea – Most Common Symptom
- Pleuritic Chest Pain
- Cough
- Wheezing
- Hemoptysis
- Tachypnea
- Tachycardia
- Fever
- Symptoms of DVT
Wells Score
- Predicts Probability of PE
- Factors:
- Physical Findings of DVT – 3 Points
- No Better Alternative Diagnosis – 3 Points
- Tachycardia (HR > 100) – 1.5 Points
- Immobilization (≥ 3 Days) or Recent Surgery (< 4 Weeks) – 1.5 Points
- History of DVT/PE – 1.5 Points
- Hemoptysis – 1 Point
- Malignancy – 1 Point
- “Traditional” Wells Interpretation:
- > 6: High Probability
- 2-5: Moderate Probability
- 0-1: Low Probability
- “Modified” Wells Interpretation:
- > 4: PE Likely
- ≤ 4: PE Unlikely
Diagnosis
- Dx: CT Pulmonary Angiogram (Gold Standard)
- If Inconclusive or Not Available Consider Ventilation-Perfusion Scan
- Low-Moderate Probability: Consider D-Dimer First
- PE Likely Excluded if D-Dimer < 500 ng/mL & Would Not Need CT
- If Unstable & High Clinical Probability: Empirically Treat Before Definitive Diagnosis
- ABG Findings:
- Hypoxemia
- Respiratory Alkalosis
- Widened Alveolar-Arterial Oxygen Gradient
- Classic ECG Findings:
- Tachycardia – Most Common EKG Finding
- S1Q3T3 Pattern (Indicates Right Ventricle Strain) – Rarely Seen
- T1-4 Inversion
- Echo Findings:
- Left Ventricle – Small but Normal Systolic Function
- Septal Flattening (RV Pressure Overload)
- Right Ventricle – Severely Dilated with Reduced Systolic Function/Wall Hypokinesis
- Pulmonary Artery Hypertension
- McConnell Sign – RV Dysfunction with Akinesia of Mid-Free Wall but Normal Motion at the Apex
- D-Sign – Left Ventricle is “D” Shaped Due to Flattening of the Interventricular Septum from Right Ventricular Overload
- D-Dimer Highly Sensitive but Not Specific
Treatment
- Stable: Anticoagulation
- Unstable & High Probability: Systemic Thrombolytics
- If Contraindicated: Embolectomy (Surgical or Endovascular)
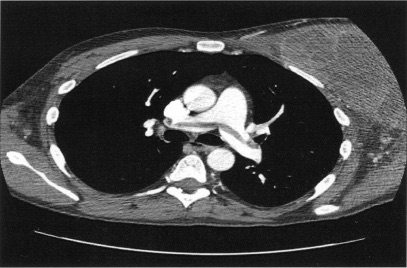
Saddle Pulmonary Embolism 1
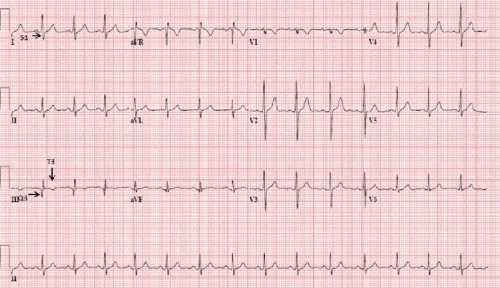
S1Q3T3 on EKG 2
References
- Daher IN, Bathina JD, Bukhari FJ, Yusuf SW. Saddle pulmonary embolism with normal right ventricular function: a treatment enigma. JRSM Short Rep. 2010 Jun 30;1(1):12. (License: CC BY-NC-2.0)
- Arshad H, Khan RR, Khaja M. Case Report of S1Q3T3 Electrocardiographic Abnormality in a Pregnant Asthmatic Patient During Acute Bronchospasm. Am J Case Rep. 2017 Feb 1;18:110-113. (License: CC BY-NC-ND-4.0)