Urology: Renal Cell Carcinoma (RCC)
Renal Cell Carcinoma (RCC)
Basics
- Most are Sporadic (4-6% Familial)
- More Common in Older Adults (55-75 Years)
- Most Common Mets: Lung
- 1/3 Have Metastases at Diagnosis
- 20-40% of Localized Disease at Diagnosis Eventually Develop Metastases
- Strongest Predictors of Malignancy:
- Male Sex
- Increase in Tumor Size
Symptoms
- Classic Triad (Rarely Seen):
- Flank Pain
- Palpable Mass
- Hematuria
- Most are Asymptomatic & Found Incidentally on Imaging
- 10-20% Have an Associated Paraneoplastic Syndrome
- More Common in Metastatic Disease
Risk Factors
- Tobacco – Strongest Risk Factor
- Obesity
- Hypertension
Paraneoplastic Syndromes
- Elevated Erythrocyte Sedimentation Rate (ESR) – The Most Common (50% of Paraneoplastic Syndromes)
- Hypercalcemia – From PTH Related Peptide Release
- Non-Metastatic Hepatic Dysfunction (Stauffer Syndrome)
- Hypertension – From Renin Release
- Erythrocytosis & Thrombocytosis
- Fever
- Cushing Syndrome
- Hyperglycemia
- Galactorrhea
- Clotting Disorders

Renal Cell Carcinoma Gross Specimen, Invading IVC 1
TNM Staging – AJCC 8
- TNM
| T | N | M | |
| I | Ia: ≤ 4.0 cm & Confined to Kidney Ib: > 4.0 cm, ≤ 7.0 cm & Confined to Kidney | LN+ | Mets+ |
| II | IIa: > 7.0 cm, ≤ 10.0 cm & Confined to Kidney IIb: > 10.0 cm & Confined to Kidney | ||
| III | IIIa: Extends into Renal Vein or its Segmental Branches, Invades Pelvicalyceal System or Invades Perirenal and/or Renal Sinus Fat but Not Beyond Gerota’s Fascia IIIb: Grossly Extends into the Vena Cava Below the Diaphragm IIIc: Grossly Extends into the Vena Cava Above the Diaphragm or Invades the Wall of the Vena Cava | ||
| IV | Invades Beyond Gerota’s Fascia |
- Stage
| T | N | M | |
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| III | T3 | N0 | M0 |
| T1-3 | N1 | M0 | |
| IV | T4 | Any N | M0 |
| Any T | Any N | M1 |
Diagnosis
- Primary Evaluation: CT or MRI
- > 15-20 Hounsfield Units (HU) is Indicative of RCC
- Unable to Reliably Diagnose RCC in Solitary Small Lesions – Generally Requires Resection
- Renal Mass Biopsy (RMB) May Be Considered in Select Circumstances
- Biopsy Often Avoided Due to Associated Risks:
- High Nondiagnostic Rate
- Occasional False-Negatives
- Potential for Cystic Tumor Spillage
- Biopsy Often Avoided Due to Associated Risks:
Treatment
- Primary Treatment: Surgical Resection
- Intermediate-High Risk Patients Should Be Offered Adjuvant Pembrolizumab (PD-1 Inhibitor)
- Locally Advanced RCC (Invading IVC) is Still Primarily a Surgical Disease
- Metastatic Disease:
- Nephrectomy with Mastectomy May Be Considered for Limited Metastatic Disease
- Factors Associated with Improved Outcomes After Metastasectomy:
- Complete Resection
- Solitary Metastatic Lesions
- Age < 60 Years
- Small Tumor Size
- Pulmonary Metastasis
- Metachronous Metastatic Disease
- May Consider Cytoreductive Nephrectomy Alone in Select Patients
Extent of Surgical Resection
- Indications for Partial Nephrectomy:
- Small T1a Lesions (< 4 cm)
- Solitary Kidney or Abnormal Contralateral Kidney
- Bilateral Tumors
- Preexisting Chronic Kidney Disease (CKD) or Proteinuria
- Multifocal Masses
- Other Comorbidities May Impact Future Renal Function
- Known Familial RCC
- Indications for Radical Nephrectomy:
- Central Location in Kidney
- Suspected Lymph Node Disease
- Extension into Renal Vein, IVC or Adrenal Gland
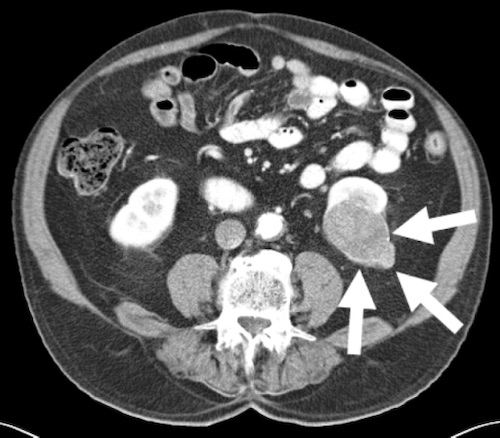
Renal Cell Carcinoma on CT 2
References
- Parissis H, Akbar MT, Tolan M, Young V. Surgical resection of a renal cell carcinoma involving the inferior vena cava: the role of the cardiothoracic surgeon. J Cardiothorac Surg. 2010 Nov 5;5:103. (License: CC BY-2.0)
- Nguyen BD, Roarke MC. Renal Cell Carcinoma with Paraneoplastic Manifestations: Imaging with CT and F-18 FDG PET/CT. Radiol Case Rep. 2015 Dec 7;2(3):72. (License: CC BY-NC-ND-4.0)