Small Intestine: Small Intestine Diverticula
Small Intestine Diverticulosis
Description
- False Diverticulum
- Herniate on the Mesenteric Border Near Arterial Entrance
Locations
- Duodenum – Most Common (45-80%)
- Most Common at 2nd Portion Near Ampulla
- Usually Solitary
- Jejunum – Second Most Common
- Commonly Multiple
- Ileum
- Commonly Multiple

Duodenum Diverticulum on EGD 1
Presentation
- Mostly Asymptomatic (90%)
- Sx: Abdominal Pain, Nausea, Vomiting & Diarrhea
- Perforation
- Bleeding
- Lemmel Syndrome
Treatment
- ASx: Observe
- Sx: Diverticulectomy
- If Second Portion of the Duodenum with Cholangitis/Pancreatitis: ERCP with Sphincterotomy/Stent & Diverticulectomy When Resolved
- Consider Prophylactic Cholecystectomy for Duodenal Diverticula
- Consider Segmental Resection of Jejunoileal Diverticula if Necessary

Duodenum Diverticulum on CT 2
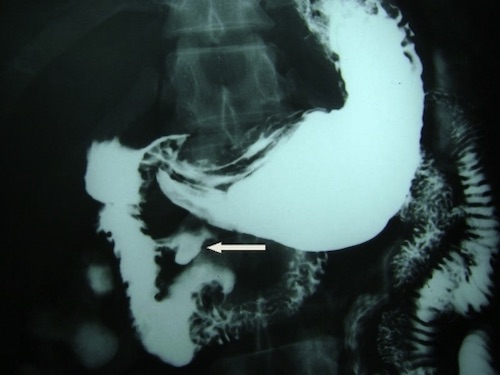
Duodenum Diverticulum on UGI 2
Meckel’s Diverticulum
Pathology
- Remnant of a Persistent Vitelline Duct Due to Failure of Obliteration
- The Most Common Congenital Small Bowel Abnormality
- Most Common Cause of Painless GI Bleed in Peds
- Most Common Neoplasia: Carcinoid
Description
- True Diverticulum
- Herniate on the Antimesenteric Border
Heterotopic Tissue
- Gastric Tissue (Most Common – 75%)
- Most Likely to Produce Sx
- Causes Bleeding
- Pancreatic Tissue (15%)
- Causes Inflammation
Presentation
- Bleeding – Most Common Presentation
- From Ulceration on the Mesenteric Border
- Ulcer Caused by Acid Produced by Ectopic Gastric Tissue
- Obstruction
- Causes: Intussusception, Volvulus, Torsion, Littre’s Hernia
- Meckel’s Diverticulitis
- Inflammation from Luminal Obstruction
- Causes: Foreign Body, Enterolith, Inflammatory Tissue or Tumor
Rules of 2’s
- 2 Feet from Ileocecal Valve
- 2 Inches Long
- 2 cm Diameter
- 2% of the Population
- 2x as Common in Males
- Most Often Presents by 2 Years Old, But Can Be Seen in Adults
- 2% Become Symptomatic
- 2 Presentations (Bleeding or Obstruction)
- 2 Types of Tissue
Diagnosis
- Meckel’s Scintigraphy Scan (99Tc)
- Detects Gastric Mucosa
- Does Not Detect Pancreatic Tissue or Hemorrhage
- 85% Sensitive in Pediatric Patients
- Much Less Sensitive in Adults (Due to Atrophic Gastric Mucosa)
Treatment
- Incidental
- On Imaging: Observation
- Intraoperative: Observation
- Possible Indication for Surgery if Found Incidentally:
- Length > 2 cm
- Palpable Abnormality
- Fibrous Bands
- Surgical Options:
- Diverticulectomy Generally Preferred
- Consider Segmental Resection if Broad Base (> 2 cm) or Palpable Abnormality at the Base
- *Historically Diverticulectomy was Dogma but Newer Evidence Recommends Observation for Most Incidental Meckel’s
- Possible Indication for Surgery if Found Incidentally:
- Diverticulitis
- Uncomplicated: Diverticulectomy
- Complicated: Segmental Resection
- Indications:
- Perforated
- Base Inflamed
- Wide Base (> 1/3 Diameter of Bowel or Neck > 2 cm)
- Indications:
- Bleeding: Diverticulectomy vs Segmental Resection
- Reason for Segmental Resection: Ulcer on Mesenteric Border & Occasionally Distal to the Antimesenteric Diverticulum
- *Historically Segmental Resection was Dogma but Newer Evidence Questions Diverticulectomy for Bleeding Meckel’s with Rare Incidence of Repeat Bleeding

Meckel Diverticulum 3
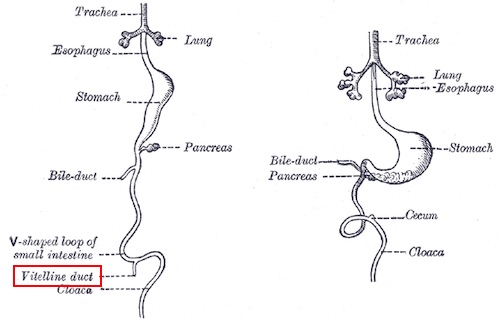
Vitelline Duct 4
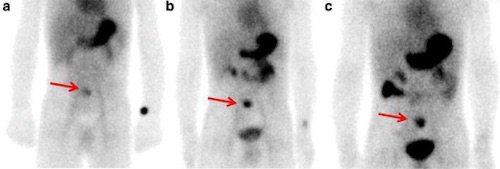
Meckel’s on Scintigraphy 5
References
- Kim PS, Jung EJ, Bang HY. Small bowel diverticulosis in patient with early gastric cancer. Ann Surg Treat Res. 2014 Oct;87(4):209-12. (License: CC BY-NC-3.0)
- Seneviratne SA, Samarasekera DN. Massive gastrointestinal haemorrhage from a duodenal diverticulum: a case report. Cases J. 2009 Jul 2;2:6710. (License: CC BY-2.0)
- Dimitriou I, Evaggelou N, Tavaki E, Chatzitheoklytos E. Perforation of Meckel’s diverticulum by a fish bone presenting as acute appendicitis: a case report. J Med Case Rep. 2013 Oct 2;7:231. (License: CC BY-2.0)
- Gray H. Anatomy of the Human Body (1918). Public Domain.
- Xie Q, Ma Q, Ji B, Gao S, Wen Q. Incremental value of SPECT/CT in detection of Meckel’s diverticulum in a 10-year-old child. Springerplus. 2016 Aug 5;5(1):1270. (License: CC BY-4.0)