Small Intestine: Ostomy
Ostomy
Definitions
- Ostomy: Surgically Created Anastomosis of the GI Tract & Skin to Allow Fecal Diversion
- Stoma: Physical End of Bowel Protruding Through the Abdominal Wall
Descriptions
- Bowel Segment
- Ileostomy: Segment of Ileum Used for Ostomy
- Output Character: Higher with Liquid Contents
- Colostomy: Segment of Colon Used for Ostomy
- Output Character: Foul-Smelling Feculent Contents
- Ileostomy: Segment of Ileum Used for Ostomy
- Bowel End
- Loop-Ostomy: A Loop of Bowel Brought to the Skin with Two Openings (One Proximal & One Distal)
- Defunctionalized Distal Limb: Proximal Functional Limb Everted to Occupy the Majority of the Aperture & Distal Limb Not Everted
- Double Barrel: Both Limbs Everted to Occupy Similar Spaces
- End-Ostomy: A Single End of Bowel is Brought to the Skin for Drainage
- Loop-Ostomy: A Loop of Bowel Brought to the Skin with Two Openings (One Proximal & One Distal)
- Permanence
- Permanent: No Plans for Later Takedown
- Permanent Colostomy Preferred Over Permanent Ileostomy if Able (Lower Risk of Dehydration & Electrolyte Abnormalities)
- Temporary/Diverting: Used to Allow Healing of Distal Site Due to High-Risk Anastomosis, Injury or Wound with Plans for Later Takedown
- Temporary Loop-Ileostomy Preferred Over End-Ostomy if Able (Easier Future Takedown)
- Permanent: No Plans for Later Takedown
Site Selection
- General Site:
- 4-5 cm Site
- Just Inferolateral to the Umbilicus on Either Side
- “Ostomy Triangle”:
- Umbilicus
- Pubic Tubercle
- ASIS
- Within Rectus Abdominis Muscle Preferred (Provides Support & Stability)
- Possibly Elsewhere Dependent of Body Habitus – Obese Are Better Suited in the Upper Abdomen
- Considerations:
- Patient Must Be Able to Visualize & Access the Stoma Easily
- Obese Often Require Placement Higher Above the Umbilicus
- Ostomy Site Must Be Flat to Avoid Interference of Appliance Adherence
- Avoid Creases, Folds, Beltline, Previous Incisions, Umbilicus & Bony Prominences
- Ensure ≥ 2 Inch Perimeter of Clear Intact Skin for Stoma Appliance Application
- Patient Must Be Able to Visualize & Access the Stoma Easily
Procedure
- Mobilize the Bowel
- Options to Gain Length:
- Release Any Bowel Adhesions
- Score Peritoneum of Mesentery (Pie-Crust)
- Divide Mesentery/Blood Supply Proximally – First Ensure that there are Adequate Distal Arcades to Supply Blood for the Ostomy
- Mobilize Peritoneal Attachments
- Transect the IMA Proximal to the Left Colonic Artery Origin
- Options to Gain Length:
- Create the Skin Opening at the Selected Site
- Consider Placing Prophylactic Mesh (Debated)
- Deliver Bowel Segment Through the Opening
- Close Remaining Abdominal Incisions
- “Mature” the Ostomy
- End-Ostomy:
- Open the Bowel
- Place Four Stay-Sutures
- Place Brooke Sutures Throughout to Evert
- Ileostomy: 3 cm Proximal Seromuscular Bite
- Colostomy: 1-2 cm Proximal Seromuscular Bite
- Loop-Ostomy:
- Consider Placing an Ostomy Bridge
- Transect 80% of the Circumference of Bowel at Antimesenteric Side
- Secure Limbs to the Abdominal Wall
- Defunctionalized Distal Limb
- Distal Limb Secured without Everting (Full-Thickness Bowel to Dermis)
- Proximal Limb Secured & Everted (Brooke Sutures)
- Double Barrel – Both Limbs Everted
- Defunctionalized Distal Limb
- End-Ostomy:
- Place an Ostomy Appliance Over the Stoma
The Difficult Ostomy – Options if Difficult to Reach
- Always Mark Site Beforehand (Obese Require a More Cephalad Site)
- Fully Mobilize (Splenic Flexure, Lateral Attachments, Omental Attachments, Retroperitoneal Attachments)
- Vessel Division:
- Divide IMA Close to its Base
- Divide IMV Just Lateral to the Ligament of Treitz
- “Pie Crust” Mesentery – Creating Sequential “Windows” within the Mesentery
- Ensure Trephine/Opening is Large Enough
- Consider a “Loop-End” Ostomy if the End Will Still Not Reach – Closed Blind End is Just Under the Skin if a Point a Few cm More Proximal Has Better Reach
- Also Known as an “End-Loop” or “Pseudo-Loop”
- Subcutaneous Lipectomy – Remove Subcutaneous Fat & Fix Skin to the Fascia
Ostomy Bridge (Stoma Rod)
- A Bar Placed Under a Loop-Ostomy to Stabilize at the Skin While Ostomy Granulates
- Removed After 3-5 Days
- Outcomes:
- No Evidence of Reduced Risk of Stoma Retraction
- Increased Risk of Local Complications (Edema, Skin Necrosis, Irritant Dermatitis, Peristomal Abscess & Bleeding)
Takedown/Reversal
- Minimum Time to Closure: 6-12 Weeks (12 Preferred)
- Allows Resolution of Acute Inflammation & Dense Adhesions
- If Protecting a Distal Anastomosis: Obtain a Contrast Enema or Flexible Sigmoidoscopy Prior to Reversal to Ensure Anastomosis is Intact
- Technique
- End-Ostomy Will Require Bowel Anastomosis to Reestablish Continuity
- Loop Ostomy is Done through a Peristomal Circumferential Incision & Closed Transversely
- Use Sharp Dissection & Avoid Serosal Tears from Blunt Dissection
Ostomy Complications
General
- Highest Overall Complication Rates: Loop-Ileostomy
- Most Common Complications: Dehydration & Skin Irritation
High-Ostomy Output
- Definition: > 1,500 cc/Day Output
- Normal Output: 600-1,200 cc/Day
- Risk After Ostomy Creation: 16-31%
- Risk Factors:
- Short Bowel
- Sepsis
- Diabetes
- Medications/Prokinetics
- Clostridioides difficile Enteritis
- Opiate Withdrawal
- Internal Fistula
- Small Bowel Diverticula
- Intermittent/Partial Obstruction (Stricture) with Bacterial overgrowth
- Management:
- Initial Management Consists of Fluid Resuscitation & Electrolyte Replacement Due to Excessive Losses
- First-Line: Soluble Fiber Supplement (Psyllium/Metamucil)
- Absorbs Water to Slow Transit Time
- *Avoid Insoluble Fiber Supplements (Wheat Bran) – Can Speed Up Transit Time
- Second-Line: Antimotility Drugs
- Loperamide (Imodium) – Generally Preferred First Medication (Lower Side Effects)
- Diphenoxylate-Atropine (Lomotil)
- Tincture of Opium
- Codeine
- Other Options:
- Octreotide
- Cholestyramine
- PPI/H2-Blockers – Anti-Secretory
- Persistent Difficulty May Be Considered for Early Ostomy Reversal if Appropriate
Stomal Ischemia/Necrosis
- Risk Factors:
- Tension
- Inadequate Blood Supply
- Inadequate Size of Opening
- Emergency Setting
- Obesity
- IBD
- Must Evaluate Extent of Necrosis
- Test-Tube Evaluation: Test Tube Inserted in Stoma & Flashlight Directed Through
- Endoscopic Evaluation: Anoscope or Flexible Sigmoidoscopy
- Tx:
- Superficial to Fascia: Observe & Reevaluate
- Extends to Fascia: Immediate Surgical Revision
- Risk Necrosis with Potential Stool Spillage
Stomal Retraction
- Definition: Stoma ≥ 0.5 cm Below the Skin Surface
- Risk Factors:
- Obesity
- Tension
- Initial Stoma Height < 1 cm
- Ileostomy More Concerning Than Colostomy with Concern for High Output Leakage
- Tx:
- Stays Above the Fascia: Local Wound Cares
- Retracted Below the Fascia: Surgical Revision
Stomal Stenosis
- Definition: Narrowing of the Stoma that Impairs Normal Function
- May Cause Cramping Pain Followed by Explosive Output
- Risk Factors:
- Peristomal Sepsis
- Stomal Retraction
- Poor-Fitting Appliance System
- Poor Surgical Technique
- Treatment:
- Asymptomatic: Dietary Modifications, Laxatives & Stool Softeners
- Symptomatic: Surgical Revision
- Preferred Approach: Local Revision with Skin Excision and Rematuring
- Consider Reseating at Another Site if Surrounding Skin is Poor or there is a Significant Parastomal Hernia
Parastomal Hernia
- Most Common After: End Colostomy
- Least Common After: Loop Ileostomy
- *May Be Due to Their Frequently Temporary Nature
- Most Develop in the First 2 Years
- Only 20% Progress to Requiring Repair
- Risk Factors:
- Obesity
- Poor Muscle Tone
- Chronic Cough
- Placement Outside of Rectus Muscle
- Large Fascial Opening
- Mesh at Index Operation Decreases Risk
- Tx:
- Electively Takedown if Able
- ASx or Mild Sx: Conservative Management (Stoma Belt (Ostomy Binder) & Weight Loss)
- Moderate-Severe Sx: Mesh Repair
- If Having Stoma Issues (Narrowing/Skin Excoriation): Relocate Stoma with Added Mesh
- Mesh Repairs
- Sugarbaker Mesh Repair
- Bowel is Secured to the Anterior/Lateral Abdominal Wall
- Intraperitoneal Mesh is then Placed Over the Bowel Loop, Circumferentially Covering the Entire Fascial Defect
- Keyhole Technique
- A 2-3 cm Keyhole is Cut-Out from the Center of the Mesh
- Intraperitoneal Mesh is then Secured Around the Bowel to Cover the Entire Fascial Defect
- Sugarbaker Mesh Repair
Stomal Prolapse
- Most Common After: Loop Transverse Colostomy
- Tx:
- Electively Takedown if Able
- Uncomplicated: Conservative Management (Cool Compress, Sugar & Manual Reduction)
- Complicated: Surgical Revision

Stomal Ischemia

Stomal Necrosis

Parastomal Hernia 1
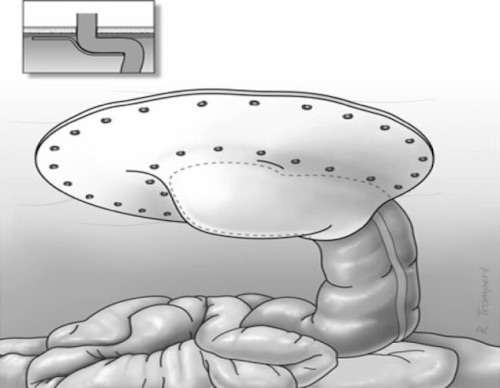
Sugarbaker Mesh Repair 2