Surgical Critical Care: Tachyarrhythmia
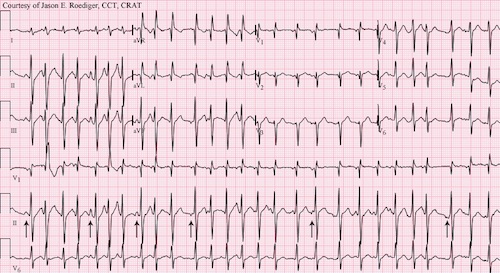
Atrial Fibrillation (A-Fib)
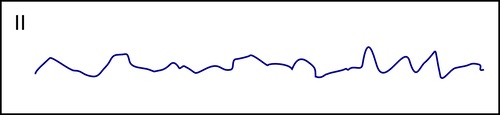
EKG Pattern
- RR-Interval with No Regular Pattern (“Irregularly Irregular”)
- No Distinct P Waves
Types
- Paroxysmal: Resolves Spontaneously
- Recurrent: ≥ 2 Episodes
- Persistent: Present for ≥ 7 Days
- Permanent: Present for ≥ One Year
General Thoughts
- The Most Common Cardiac Arrhythmia
- Most Common Cause Postop: Fluid Overload
- Increases Risk for Thromboembolism Formation within the Left Atrium
- Risk for Stroke or Other Ischemic Events
Treatment
- Acute Treatment:
- Stable: Rate Control (*See Below)
- β-Blockers
- Generally Preferred in Hyperadrenergic States (Acute MI or Postop)
- Contraindicated in COPD or CHF
- Metoprolol Boluses or Esmolol gtt
- Diltiazem – Generally Superior to Amiodarone
- Amiodarone – Favored Agent in Concomitant Heart Failure
- Digoxin – Only an Adjunct, Not Sole Therapy
- β-Blockers
- Unstable: Synchronized Cardioversion
- Stable: Rate Control (*See Below)
- Chronic Treatment: Rate Control Generally Preferred
- Anticoagulation Indications:
- Postoperatively Persists > 48 Hours
- If Requires Cardioversion
- CHADS-VASC Score ≥ 1-2
- CHF History (+1)
- HTN History (+1)
- Age ≥ 65 (+1) or ≥ 75 (+2)
- DM History (+1)
- Stroke/TIA/Thromboembolism History (+2)
- Vascular Disease History (MI, PAD or Aortic Plaque) (+1)
- Sex Female (+1)
General Treatment Goals
- Chronic Setting: < 110 bpm
- Acute Setting: < 110-120 bpm (Less Well Defined)

Atrial Fibrillation 1
Other Tachyarrhythmia
Sinus Tachycardia (ST)
- EKG Pattern:
- Heart Rate > 100 bpm
- Normal P Waves Preceding Every QRS Complex
- Compared to SVT:
- Most Likely Secondary to Underlying Cause (Pain/Stressor)
- Progressively Increases Rate
- HR Usually Not Very High < 150 bpm
- Typically See Separate P & T Waves
- Generally Asymptomatic
- May See Moderate Rate Variability
- Treatment: Treat Underlying Cause
- Indications for β-Blocker Treatment:
- Acute Coronary Syndrome
- Symptomatic Inappropriate (No Explanation) Sinus Tachycardia
- Indications for β-Blocker Treatment:
Atrial Flutter
- EKG Pattern:
- Rapid Regular Atrial Depolarizations (“Saw Tooth” Pattern) – About 300 bpm
- Not All P Waves Produce a Ventricular Contraction
- Regular Ventricular Rate – About 150 bpm
- Treatment: Similar to Atrial Fibrillation
Multifocal Atrial Tachycardia (MAT)
- EKG Pattern:
- “Chaotic” Variable P Waves with ≥ 3 Different Morphologies (Different Sites of Origin)
- Heart Rate > 100 bpm
- Strongly Associated with Pulmonary Disease (COPD Most Common)
- Also Seen in Cardiac Disease, Hypokalemia or Hypomagnesemia
- Treatment:
- First Step: Correct Hypomagnesemia & Hypokalemia
- If Serum Magnesium Normal: Give Empiric Magnesium
- MgSO4 Bolus 2 g, Then Infuse 6 g Over 6 Hours
- If Fails: Metoprolol
- Severe Bronchospasm: Verapamil
Supraventricular Tachycardia (SVT)/Paroxysmal Supraventricular Tachycardia (PSVT)
- EKG Pattern:
- Heart Rate > 100 bpm
- Narrow QRS Complex (< 120 ms)
- Compared to Sinus Tachycardia:
- Often Has No Identified Underlying Cause
- Sudden Onset
- HR Usually Very High > 150 bpm
- Typically See Combined P & T Waves
- Generally Symptomatic
- Often Has Limited Rate Variability
- Types:
- Atrioventricular Nodal Reentrant Tachycardia (AVNRT) (60% – Most Common)
- Atrioventricular Reentrant Tachycardia (AVRT) (30%)
- Sinoatrial Nodal Reentry Tachycardia (SNART)
- Focal Atrial Tachycardia
- Junctional Ectopic Tachycardia
- Treatment:
- Stable:
- Initial: Vagal Maneuvers (Carotid Massage & Valsalva Maneuver)
- 12-18% Success
- If Fails: Adenosine
- Initial: Vagal Maneuvers (Carotid Massage & Valsalva Maneuver)
- Unstable: Synchronized Cardioversion
- Stable:
Wolff-Parkinson-White Syndrome (WPW)
- EKG Pattern:
- Pre-Excitation “Delta Waves” (Slurring Slow Risk of the Initial QRS Complex)
- Short PR Interval (< 120 ms)
- Prolonged QRS Complex
- Accessory Pathway Through the Bundle of Kent
- May Cause Recurrent SVT
- Treatment:
- Stable: Procainamide
- Avoid Drugs that Block AV Node (β-Blockers, CCB & Digoxin) – Can Cause Conversion to VT/VF
- Unstable: Synchronized Cardioversion
- Stable: Procainamide
Ventricular Tachycardia (VT)
- EKG Pattern:
- Heart Rate > 100 bpm
- Wide QRS Complex (≥ 120 ms)
- No Fixed Relationship of P Wave & QRS Complex
- If Sustained (> 30 Seconds) There Can Be an Immediate Threat to Life
- Treatment:
- Stable: Amiodarone
- Unstable: Synchronized Cardioversion
Torsades de Pointes
- EKG Pattern:
- Polymorphic Ventricular Tachycardia
- QRS Complexes Appear to Be “Twisting Around the Isoelectric Points”
- Associated with Prolonged QT Intervals
- Can Convert to Ventricular Fibrillation
- Treatment: IV Magnesium
- MgSO4 Bolus 2 g, Then Infuse 2-4 mg/min
Ventricular Fibrillation (VF)
- EKG Pattern:
- Sudden Chaotic Irregular Deflections
- No Identifiable P Waves, QRS Complexes or T Waves
- Rate 150-500 bpm
- Non-Perfusing Rhythm
- Fatal if Not Corrected
- Treatment:
- Initial: Start CPR & Give Oxygen
- Every 2 Minutes:
- Check Rhythm
- Defibrillation
- Alternate Epinephrine & Amiodarone Every Other 2 Minutes

Sinus Tachycardia 1

Atrial Flutter 1
Multifocal Atrial Tachycardia 2

Supraventricular Tachycardia 3
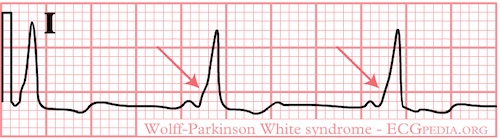
Wolff-Parkinson-White Syndrome 1
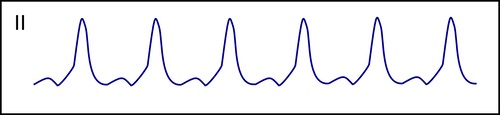
Ventricular Tachycardia 1
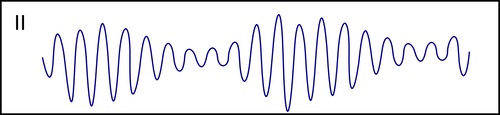
Torsades de Pointes 1
Ventricular Fibrillation 1
Antiarrhythmic Pharmacology
Antiarrhythmic Pharmacology
References
- ECGPedia.org. (License: CC BY-SA-3.0)
- Jer5150. Wikimedia Commons. (License: CC BY-SA-3.0)
- Wikimedia Commons. (License: Public Domain)