Urology: Testicular Cancer
Testicular Cancer
Types
- Germ Cell Tumors (95%)
- Seminoma (Most Common)
- Nonseminomatous
- Teratoma
- Choriocarcinoma
- Embryonal Carcinoma
- Yolk Sac
- Stromal Tumors (5%)
- Leydig Cell Tumor (Most Common)
- Sertoli Cell Tumor
- Granulosa Cell Tumor
- Other Tumors
- Lymphoma
- Carcinoid
- Metastases
Risk Factors
- Germ Cell Tumors:
- Cryptorchidism
- Infertility
- Hypospadias
- HIV
- Stromal Tumors:
- No Known Risk Factors
Prognosis
- Most Common Solid Malignancy in Males Age 15-35
- High Survival Rate Due to Modern Advances – Previously was the Most Common Cancer-Related Death in Males Age 25-35
- Seminomas are Exquisitely Sensitive to Radiation Therapy with a Favorable Prognosis
- Embryonal Carcinomas are Aggressive with High Rates of Metastases
Presentation
- Painless Nodule/Mass
- Heavy Sensation
- Dull Ache
- Gynecomastia from hCG Production
- Symptoms from Metastases
- Leydig Cell Tumors May Present with Precocious Puberty, Virializing or Feminizing Due to Testosterone Production
Diagnosis
- Initial Evaluation: US & Serum Tumor Markers
- Serum Tumor Markers: AFP, Beta-HCG & LDH
- Check Hormonal Markers if Stromal Tumor Suspected: Testosterone, LH & FSH
- CT of Chest/Abdomen/Pelvis for Staging
- Definitive Diagnosis: Pathology on Orchiectomy
- Do Not Biopsy – Risk for Tumor Seeding to Scrotal Sac & Metastatic Spread to Inguinal Nodes
Serum Tumor Markers
- Seminoma: Beta-HCG & LDH May Be High
- AFP Not Elevated
- Nonseminomatous Germ Cell Tumors: AFP, Beta-HCG & LDH May Be High
- Stromal Tumors: Negative Tumor Markers
- May See Elevation of Hormonal Markers
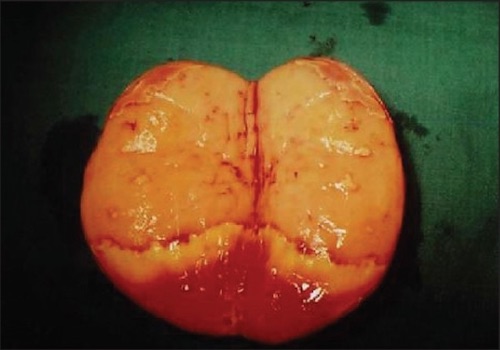
Seminoma, Testicle Opened After Resection 1
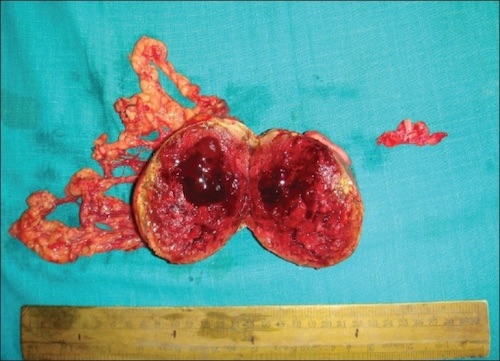
Embryonal Carcinoma, Testicle Opened After Resection 2
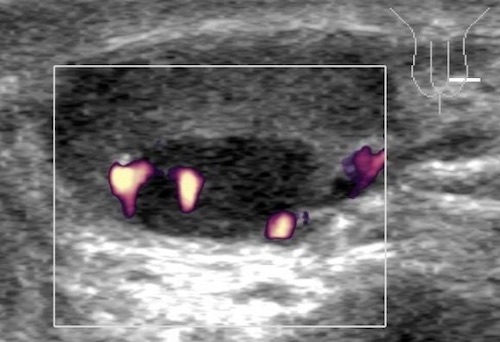
Seminoma US 3
TNM Staging – AJCC 8
- TNM
| T | N | M | |
| I | Confined to Testicle | 1-5 LN ≤ 2 cm | Mets+ |
| II | Invaded Blood Vessels, Lymphatics, Epididymis, Fatty Tissue or Tunica Vaginalis | > 5 LN or 2-5 cm | |
| III | Invaded the Spermatic Cord | LN > 5 cm | |
| IV | Invaded the Scrotum |
- Stage
| T | N | M | |
| I | Any T | N0 | M0 |
| II | Any T | N1 | M0 |
| III | Any T | Any N | M1 |
- Staging Subgroups Include Serum Tumor Markers (S) – LDH, Beta-HCG & AFP
Treatment
- Primary Treatment: Radical Orchiectomy by Inguinal Incision
- Inguinal Incision Avoids the Lymphatics of a Scrotal Approach
- May Consider Partial Orchiectomy if Polar Mass ≤ 2 cm & Abnormal or Absent Contralateral Testicle
- Retroperitoneal Lymph Node Management:
- Seminoma: Radiation Therapy
- Nonseminomatous or Stromal Tumor: Retroperitoneal Lymph Node Dissection (RPLND)
- *Consider Active Surveillance Alone for Stage I with Low Risk for Recurrence
- Advanced Disease: Chemotherapy
Radical Orchiectomy – Procedure
- Inguinal Incision & Incise External Oblique Fascia (Similar to Inguinal Hernia)
- Mobilize Cord (Preserve Ilioinguinal Nerve)
- Divide External Spermatic Fascia & Cremasteric Fibers
- Deliver Testicle by Gentle Cephalad Traction
- Mobilize Cord to Level of Internal Ring
- Individually Dissect, Ligate & Divide the Vas Deferens & Gonadal Vessels
- High-Ligation at Level of Internal Inguinal Ring (Key Step)
- Closure
References
- Agrawal S, Bajpai R, Agrawal RK, Gupta TC. Bilateral synchronous seminoma with bilateral cryptorchidism of the testis. Indian J Urol. 2010 Oct;26(4):587-9. (License: CC BY-NC-SA-3.0)
- Barmon D, Kataki AC, Sharma JD, Hafizur R. Embryonal carcinoma in androgen insensitivity syndrome. Indian J Med Paediatr Oncol. 2011 Apr;32(2):105-8. (License: CC BY-NC-SA-3.0)
- Dieckmann KP, Anheuser P, Sattler F, Von Kügelgen T, Matthies C, Ruf C. Sequential bilateral testicular tumours presenting with intervals of 20 years and more. BMC Urol. 2013 Dec 9;13:71. (License: CC BY-2.0)