Endocrine: Thyroidectomy
Thyroidectomy
Positioning
- Arms Tucked
- Neck Extended
Procedure
- Identify the Thyroid:
- Transverse “Kocher Incision”
- 1-2 Fingerbreadths Above Sternal Notch
- Traditionally 8-10 cm Long – Generally Shorter (5-6 cm) in Modern Practice
- Divide Platysma
- Superior Subplatysmal Flap Carried to Cricoid Cartilage
- Inferior Subplatysmal Flap Carried to Sternal Notch
- Divide Midline Raphe (Avascular Plane Between Strap Muscles)
- Transverse “Kocher Incision”
- Expose One Thyroid Lobe:
- Dissect the Entire Anterior Capsule of One Thyroid Lobe from Medial to Lateral
- Thyroid Gland is Rolled Medially to Expose the Posterior Capsule
- Vessels to Ligate:
- Middle Thyroid Vein (No Middle Artery) – At the Lateral Aspect
- Superior Thyroid Vessels – To Superior Pole
- Inferior Thyroid Vessels – To Inferior Pole
- Caution:
- Ensure Meticulous Intraoperative Hemostasis
- Avoid Thyroid Capsule Rupture
- Identify & Protect the Recurrent Laryngeal Nerve in the Tracheoesophageal Groove
- Avoid Parathyroid Gland Devascularization or Resection
- Dissect the Entire Posterior Capsule from Lateral to Medial
- Medial Dissection:
- Divide the Ligament of Berry as Close to the Trachea as Possible
- Avoid RLN Injury
- Dissect the Isthmus Off the Anterior Aspect of the Trachea
- Divide the Ligament of Berry as Close to the Trachea as Possible
- Next Step:
- Thyroid Lobectomy: Divide the Thyroid at the Isthmus
- Total Thyroidectomy: Repeat Dissection on the Contralateral Side
- Finish & Close:
- Obtain Hemostasis
- Close Strap Defect
- Close Platysma Defect
- Close Skin

Thyroidectomy Incision 1
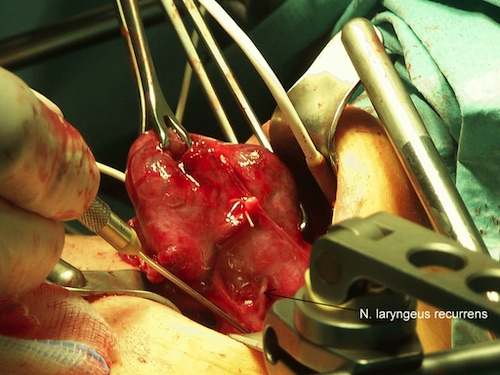
Thyroidectomy Showing Recurrent Laryngeal Nerve (Arrow) 2
Complications
Cervical Hematoma
- Risk: 0.7-1.5%
- Must Ensure Meticulous Intraoperative Hemostasis
- Even Low-Volume Bleeding Can Cause Life-Threatening Airway Obstruction
- Can Cause Airway Edema from Venous/Lymphatic Obstruction Making Intubation Difficult
- Routine Drain Placement is Unnecessary
- Generally Recommended for Persistent Oozing or Extensive Dissections
- Treatment:
- Respiratory Distress: Emergently Open at Bedside
- Not in Respiratory Distress: Intubate & Emergently Open in the OR
Nerve Injury
- Risk:
- Recurrent Laryngeal Nerve Injury: 0-11%
- Bilateral Vocal Cord Paralysis: 0.4%
- Prevention:
- Indications for Preoperative Laryngoscopy:
- Preoperative Hoarseness or Voice Changes
- History of Neck or Mediastinal Surgery
- Posterior Extrathyroidal Extension of Tumor
- Bulky Lymphadenopathy
- *Routine Assessment Unnecessary
- Intraoperative Nerve Monitoring (IONM):
- Surface Electrodes on the Endotracheal Tube Sense When the Recurrent Laryngeal Nerve is Stimulated
- Generally Recommended if There is a History of Prior Neck Surgery
- *Routine Use is Controversial
- Indications for Preoperative Laryngoscopy:
- Most Common Nerve Injury: Superior Laryngeal Nerve (SLN)
- Most Common Site of RLN Injury: Ligament of Berry
- If Recurrent Laryngeal Nerve (RLN) Transection Identified Intraoperatively: Primary Anastomosis
- May Use Ansa Cervicalis Nerve Graft to Avoid Tension
Transient Hoarseness
- Common After Thyroid Surgery
- Caused by Vocal Cord Edema from Endotracheal Intubation
- Generally Resolves After 24-48 Hours
- Persistent Hoarseness Should Raise Concern for Vocal Cord Motion Abnormality
Hypothyroidism
- Surgical Risk:
- Total Thyroidectomy: All Have Postoperative Hypothyroidism
- Lobectomy/Hemithyroidectomy: At Risk for Postoperative Hypothyroidism (Risk: 22%)
- Smaller Size Residual Thyroid Tissue Increases Risk
- Labs Should Be Drawn at 4-6 Weeks Postop to Evaluate
- Staging:
- Subclinical Hypothyroidism: Elevated TSH & Normal Free T4
- Most Often Asymptomatic
- Often Can Progress to Overt Hypothyroidism
- Overt Hypothyroidism: Elevated TSH & Low Free T4
- Mostly Symptomatic
- Subclinical Hypothyroidism: Elevated TSH & Normal Free T4
- Treatment: Thyroid Hormone (Levothyroxine) Replacement
- Subclinical Cases After Hemithyroidectomy Should Still Be Treated Even if Asymptomatic
- Patients After Total Thyroidectomy will Require Lifelong Hormone Replacement
Hypoparathyroidism
- Transient Hypoparathyroidism/Hypocalcemia (1-49%)
- Common Even When Parathyroid Glands are Meticulously Preserved
- Liberal Use of Calcium & Vitamin D Supplementation Encouraged After Total Thyroidectomy
- Permanent Hypoparathyroidism (2%)
- From Inadvertent Parathyroid Gland Devascularization or Resection
References
- Wikimedia Commons. (License: Public Domain)
- THWZ. Wikimedia Commons. (License: CC BY-SA-3.0)