Trauma: Traumatic Brain Injury (TBI)
Traumatic Brain Injury (TBI)
General
- Causes:
- Most Common Leading to Hospitalization: MVC
- Most Common Leading to Death: GSW
- Most Common in Elderly: Falls
- Classification:
- Mild: GCS 13-15
- Moderate: GCS 9-12
- Severe: GCS ≤ 8
- Coagulopathy Develops from Tissue Thromboplastin Release
Epidural Hematoma (EDH)
- Bleeding Between the Dura Mater & Skull
- Most Common Source: Middle Meningeal Artery
- Associated with Temporal Fractures
- CT Appearance: Lentiform/Biconvex, Does Not Cross Midline
- “Lucid Interval” – A Relatively Normal Period of Time from the Initial Concussion to Subsequent Coma
Subdural Hematoma (SDH)
- Bleeding Between the Dura Mater & Arachnoid Mater
- Most Common Intracranial Hemorrhage
- Source: Venous Plexus/Bridging Veins
- Acceleration/Deceleration Injury
- CT Appearance: Crescent, Crosses Midline
- Can Be Chronic in Elderly After Falls
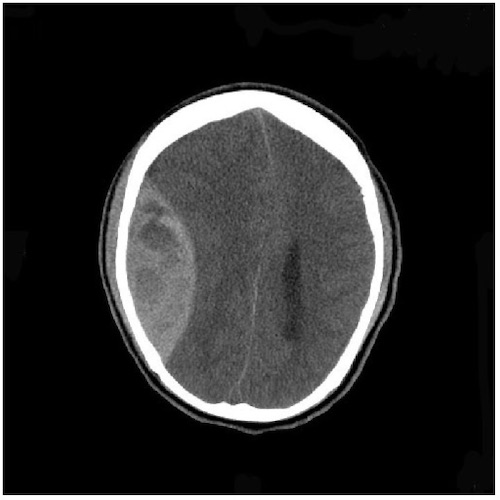
EDH 1

SDH 2
Subarachnoid Hemorrhage (SAH)
- Bleeding Between the Brain & Arachnoid Mater
- Causes:
- Trauma #1
- Aneurysm #2
- Arteriovenous Malformation (AVM)
- “Thunderclap” Headache that is “Worst of Life”
- Xanthochromia of CSF (Pathognomonic) – Yellow Coloring
- Only if Neurologically Intact
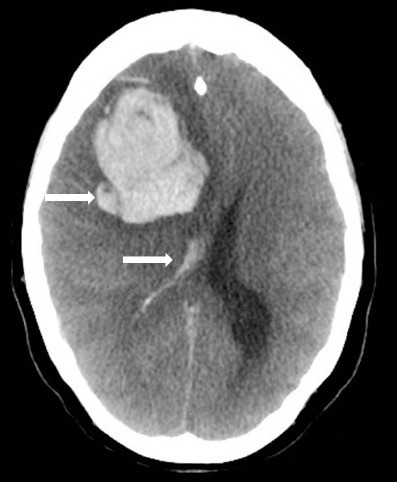
SAH 3

Xanthochromia 4
Diffuse Axonal Injury (DAI)
- A Diffuse Shearing Injury of Brain Axons
- Most Common Cause: Rotational Force of Acceleration/Deceleration Impact
- May Not Be Apparent on CT
- MRI Appearance:
- Punctate Hemorrhages
- Blurring of Grey-White Interface
- Very Poor Prognosis
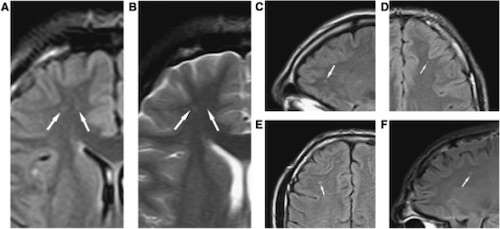
DAI on MRI 5
Cerebral Contusion (Parenchymal/Hemorrhagic Contusion)
- Bruising of the Brain from Multiple Punctate Hemorrhages
- May See Surrounding Edema & Necrosis
- Most Remain Small & Surgically Insignificant
- Evolve Over Time – May Worsen or Not Even Be Evident on Initial CT
- Often See “Coup & Countercoup” Injuries
- “Coup” – Injury at the Site of Head Impact
- “Countercoup” – Injury Remote from the Site of Head Impact (Classically Directly Opposite)
- Most Common Sites: Frontal Base and Anterior Temporal Lobes
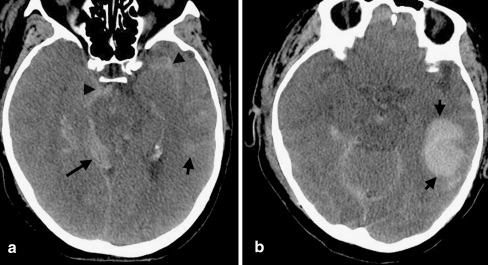
Cerebral Contusion 6
Secondary Brain Injury
- Injury That Develops After the Initial/Primary Brain Injury from Metabolic & Physiologic Derangements
- Risk Factors:
- Hypotension
- Reduced CPP Causes Ischemia
- Autoregulation with Arteriole Vasodilation Causes Increased ICP
- Doubles the Mortality
- Hypoxia
- Hypotension
Treatment
- Admit to ICU if Moderate-Severe Injury
- Seizure Prophylaxis:
- Indications: Severe TBI (Not Mild-Moderate)
- 1 Week of Levetiracetam (Keppra) or Fosphenytoin
- Reduce Risk of Early Seizures
- No Reduced Risk for Late Seizures or Post-Traumatic Epilepsy
- Surgical Decompression Indications:
- Epidural Hematoma
- > 30 cc Volume
- GCS ≤ 8 & Pupil Abnormality
- Subdural Hematoma
- > 10 mm Thick
- > 5 mm Midline Shift
- GCS ≤ 8 & Pupil Abnormality or GCS Decreased by ≥ 2
- Subarachnoid Hemorrhage
- Posterior Fossa Causing Mass Effects
- Cerebral Hemispheres > 50 cc
- Or > 20 cc with Midline Shift > 5 mm & GCS ≤ 8
- Epidural Hematoma
- Anticoagulation Management:
- If on Coumadin: Repeat CT for Possible Delayed Bleed
- Start Prophylactic Anticoagulation Within 24-48 Hours of a Stable Head CT
- *Use of Beta-Blockers to Blunt Sympathetic Activation Cascade After TBI is Evolving
Brain Injury Guidelines (BIG)
| Variables | BIG 1 | BIG 2 | BIG 3 |
| LOC | Yes/No | Yes/No | Yes/No |
| Neuro Exam | Normal | Normal | Abnormal |
| Intoxication | No | No/Yes | No/Yes |
| CAP (Coumadin, Aspirin, Plavix) | No | No | Yes |
| Skull Fracture | No | Non-displaced | Displaced |
| SDH | < 4 mm | 5-7 mm | > 8 mm |
| EDH | < 4 mm | 5-7 mm | > 8 mm |
| IPH (Locations) | < 4 mm (x1) | 5-7 mm (x2) | > 8 mm (Multiple) |
| SAH | Trace | Localized | Scattered |
| IVH | No | No | Yes |
- Management:
- BIG 1: Observe for 6 Hours
- BIG 2: Admit & Observe for 24 Hours
- BIG 3: Admit, Repeat Head CT & Consult Neurosurgery
Intracranial Pressure (ICP)
Monro-Kellie Doctrine
- The Sum of the Volumes of Brain Matter, CSF & Intracranial Blood is Constant
- An Increase in One Will Cause a Decrease in One or Both of the Others
- Therefore an Elevated ICP will Result in Decreased Cerebral Perfusion Pressure & Risk for Herniation
Values
- Intracranial Pressure (ICP)
- Normal: 10 mmHg
- Goal: < 20 mmHg
- Peaks 48-72 Hours After Trauma
- Cerebral Prefusion Pressure (CPP)
- CPP = MAP – ICP
Signs of Elevation
- Cushing’s Triad
- From Increased ICP
- Causes Increased Sympathetic & Parasympathetic Activity
- Late Sign – Suggests Impending Herniation
- Triad:
- HTN (Widened Pulse Pressure)
- Bradycardia
- Irregular Breathing Pattern
- Stages:
- First Stage
- From Increased ICP
- Increases Sympathetic Activity
- Increases BP & HR
- Second Stage
- From Aortic Arch Baroreceptors Due to HTN
- Increases Parasympathetic Activity
- Decreases HR
- Third Stage
- From High ICP, HR Changes & Endogenous Stimuli
- Distorts Brainstem Pressures
- Irregular Breathing
- First Stage
- From Increased ICP
- Uncal Herniation
- Earliest Sign: Eyes (Ptosis, Anisocoria (Unequal Pupil Size) & Impaired Movement)
- Dilated/Blown Pupil
- Indicates Pressure on Ipsilateral Oculomotor CN III
- Pain
- Double Vision (Due to CN VI Palsy)
ICP Monitors
- Indications:
- Abnormal CT & GCS ≤ 8
- Normal CT & ≥ 2 of:
- Age > 40
- Motor Posturing
- SBP < 90
- Types:
- Bolt (Codman ICP Monitor)
- Bolt Placed into the Parenchyma with Fiberoptic Monitoring of ICP
- Only Measures ICP
- External Ventricular Drain (EVD/Ventriculostomy)
- Drain Placed into the Ventricle
- Measures ICP & Allows Therapeutic CSF Drainage
- Bolt (Codman ICP Monitor)
CPP Management
- Goal CPP > 60 mmHg
- Range 50-70 mmHg
- Goal: Avoid Secondary Brain Injury
- Initial Measures:
- IVF (NS)
- Pressor Support – Avoid Hypotension
- Elevate Head-of-Bed to 30 Degrees – Allow Adequate Venous Drainage
- Sedation & Analgesia – Decrease Pain & Metabolic Demand
- Intermittent CSF Drainage
- Normothermia – Fever Increase Metabolic Demand & Blood Flow
- Avoid LP (Precipitates Herniation)
- Secondary Options:
- Osmotic Therapy (Goal Na 145-155)
- Hypertonic Saline or Mannitol Boluses (Not Continuous)
- Avoid Mannitol if Hypotensive or Hypovolemic
- Hypertonic Saline or Mannitol Boluses (Not Continuous)
- Hyperventilate (PaCO2 30-35) – Induce Cerebral Vasoconstriction
- Exchange Parenchymal Pressure Monitor to External Ventricular Drain
- Osmotic Therapy (Goal Na 145-155)
- Refractory Treatment:
- Decompressive Craniectomy
- Improved Survival but More Survivors are Dependent on Others and Higher Risk of Unfavorable Outcomes (RESCUEicp and DECRA Trials)
- Neuromuscular Paralysis
- Barbiturate Coma
- Hypothermia
- Decompressive Craniectomy
References
- Yogarajah M, Agu CC, Sivasambu B, Mittler MA. HbSC Disease and Spontaneous Epidural Hematoma with Kernohan’s Notch Phenomena. Case Rep Hematol. 2015;2015:470873. (License: CC BY-3.0)
- Choi HJ, Lee JI, Nam KH, Ko JK. Acute Spontaneous Subdural Hematoma due to Rupture of a Tiny Cortical Arteriovenous Malformation. J Korean Neurosurg Soc. 2015 Dec;58(6):547-9. (License: CC BY-NC-3.0)
- Al-Hameed FM. Spontaneous intracranial hemorrhage in a patient with Middle East respiratory syndrome corona virus. Saudi Med J. 2017 Feb;38(2):196-200. (License: CC BY-NC-SA-3.0)
- Kwon SK, Kim MW. Pseudo-Froin’s syndrome, xanthochromia with high protein level of cerebrospinal fluid. Korean J Anesthesiol. 2014 Dec;67(Suppl):S58-9. (License: CC BY-NC-3.0)
- Gandy S, Ikonomovic MD, Mitsis E, Elder G, Ahlers ST, Barth J, Stone JR, DeKosky ST. Chronic traumatic encephalopathy: clinical-biomarker correlations and current concepts in pathogenesis. Mol Neurodegener. 2014 Sep 17;9:37. (License: CC BY-2.0)
- Kim JJ, Gean AD. Imaging for the diagnosis and management of traumatic brain injury. Neurotherapeutics. 2011 Jan;8(1):39-53. (License: CC BY-NC-2.0)