Small Intestine: Small Bowel Obstruction (SBO)
Definitions & Presentation
Definitions
- Small Bowel Obstruction: Interruption of the Normal Flow of Intraluminal Contents
- Functional SBO: Dysfunctional Peristalsis
- Also Known as Ileus
- Mechanical SBO: Intraluminal or Extraluminal Compression
- “Small Bowel Obstruction” Typically Refers to a “Mechanical Small Bowel Obstruction”
- Functional SBO: Dysfunctional Peristalsis
- Partial SBO
- Some Gas or Liquid Stool is Able to Pass the Obstruction
- Complete SBO
- Nothing is Able to Pass the Site of Obstruction
- Closed Loop Obstruction
- Both Proximal and Distal Ends Obstructed
- No Outlets for Decompression
- Rapid Progression with High Risk for Strangulation & Perforation
- Both Proximal and Distal Ends Obstructed
Causes Mn
- Postoperative Adhesions – Most Common Cause in US
- Hernia – Most Common Cause in “Virgin Abdomens” (No Past Surgery) & Most Common Cause Worldwide
- Cancer – Most Common Cause of Large Intestine Obstruction (Regardless of Surgical History)
- Inflammatory Bowel Disease
- Stricture
- Intussusception
- Foreign Body
- Midgut Volvulus
- Most Common in Peds
- Rare in Adults
- Primary
- Risk Factors: Long Mesentery, Deficient Mesenteric Fat & Narrow Mesenteric Base
- Secondary (Most Common) – Due to Other Pathology (Adhesions/Malrotation)
- Primary
- Gallstone Ileus
Symptoms
- Nausea & Vomiting
- Proximal Obstructions Have More Severe N/V Than Distal Obstructions
- Intermittent Pain (Periumbilical Cramping)
- As Bowel Dilates & Pressure Overcomes Capillary Pressure Wall Ischemia Causes Peritonitis with Constant Sharp Pain
- Abdominal Distention
- Obstipation (Unable to Pass of Flatus or Stool)
- *Colon Obstruction Has Constant Pain with Feculent Emesis & Significant Distention
Diagnosis
Diagnosis
- Diagnosis: Radiology
- CT (95% Sensitive) Better Than Plain Radiography (67% Sensitive)
- Small-Bowel Follow Through (SBFT)
- Given Oral Water-Soluble Contrast (Gastrografin) & X-Ray is Taken After a Period of Time
- May Be Done at Periodic Intervals or a Single Image After a Few Hours
- Generally No Benefit Extending Past 8 Hours
- Pass if Patient Has a Bowel Movement or if Contrast is Seen in the Colon
- Bowel Must First Be Decompressed & Not Actively Vomiting
- Helps Identify Patients Unlikely to Resolve by Conservative Measures
- May Also Be Therapeutic as a Cathartic Agent – Hyperosmolar Agent to Reduce Bowel Edema & Acts as a Laxative
- Given Oral Water-Soluble Contrast (Gastrografin) & X-Ray is Taken After a Period of Time
General Radiographic Findings
- Proximal Dilated Loops > 3 cm & Distal Decompressed Loops
- Air-Fluid Levels (Air from Swallowed Nitrogen)
- “Gasless Abdomen” without Air-Fluid Levels Can Be Seen When Obstruction Causes Fluid Sequestration
- Paucity of Gas in the Colon
- Transition Point
- “Swirling” of Mesentery Suggests a Closed-Loop Obstruction
Radiographic Findings that Predict the Need for Operative Exploration
- Absence of Fecalization of the Small Bowel – Fecalization is an Abnormal Sign But is a Reassuring Finding in the Setting of SBO (Indicates that the Obstruction has Been Present Long Enough for the Stasis to Allow Fecalization to Occur)
- Mesenteric Edema
- Bowel Wall Thickening
- Free Intraperitoneal Fluid
Grade
- Definitions are Varied & With Improved CT Imaging it is More Commonly Noted
- Low-Grade SBO – Generally Describes Partial SBO without a Discrete Transition Point
- High-Grade SBO – Generally Describes Complete SBO with a Discrete Transition Point
AAST Grade
- I: Partial SBO
- II: Complete SBO; Bowel Viable & Not Compromised
- III: Complete SBO; Bowel Viable but Compromised
- IV: Complete SBO; Bowel Nonviable or Perforation with Local Spillage
- V: Perforation with Diffuse Peritoneal Contamination
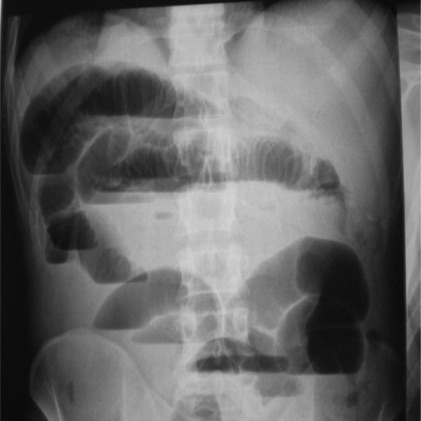
SBO on Plain Film 1
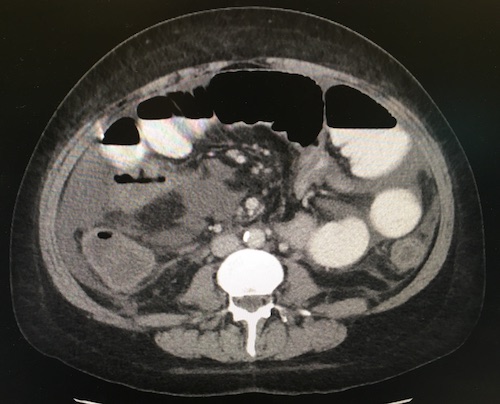
SBO on CT
Management
Initial Management
- Preferred: Conservative Management
- Immediate Surgery Indications:
- Closed-Loop
- Signs of Strangulation or Ischemia
- Perforation
- Multiple Recurrence
- *Previously Believed that All “Virgin Abdomens” (No Surgical History) with SBO Should Undergo Surgery Due to Risk of Malignancy Has Since Fallen Out of Favor – Improved CT Scans Allow for Better Recognition of Malignancy & Many Have Other Reasons for Scar Tissue that May Have Been Unrecognized
Conservative Management
- Managements:
- NPO
- IV Fluids
- Nasogastric Tube for Decompression
- Failure Duration Prior to Proceeding with Surgery: 3-5 Days (Debated)
- Success for Adhesive SBO Resolution: 65-80%
- Recurrence Rate for Adhesive SBO: 16-53%
Surgical Management
- Open Laparotomy Generally Preferred Over Laparoscopy
- Laparoscopic Indications:
- Mild Abdominal Distention (Bowel Diameter ≤ 4 cm & Early Presentation)
- Partial Obstruction
- Proximal Obstruction
- Few Operative Procedures
Adhesiolysis
- General Procedures:
- Run Bowel from Ligament of Treitz to the Ileocecal Valve
- Lysis of Adhesion (Enterolysis)
- Address Principal Site of Obstruction & Major Adhesions
- Total Lysis of All Adhesions Unnecessary & Risks Damage to Healthy Bowel
- Reduce & Repair Hernias
- Perforations:
- Serosal Injuries: Oversew to Imbricate Mucosa
- Circumference < 50%: Primary Repair
- Circumference > 50%: Resect
- Resect Nonviable Bowel
- Consider Open Abdomen with Reexploration in 24-48 Horus if Viability Uncertain
- Preform an Oncologic Resection for any Mass (5-10 cm Margin with Associated Lymph Nodes)
- Consider Manual Bowel Decompression (“Milking”) – Debated Effects
- Decompresses the Abdominal Compartment with Less Tension for Closure
- May Reduce Risk for Aspiration Pneumonia
- May Induce Paralytic Ileus Although Transit Time Generally Not Affected
- Surgical Management of Strictures:
- Single Stricture: Stricturoplasty
- Multiple Strictures: Resection
- Large Intestine: Resection
- High Malignancy Risk
Other Considerations
- Patients Admitted to a Surgical Service (Opposed to Medical Service) Have Better Outcomes
- Shorter Length of Stay
- Shorter Time to Surgery
- Lower Hospital Costs
- Lower Rate of Readmission
- Lower Mortality
- Malignant Obstruction:
- Palliative Treatment for Nausea/Vomiting: Octreotide
- Consider Palliative Bypass if Large & Unresectable
- Consider Decompressive Gastrostomy if Multiple Points of Obstruction
Mnemonics
General Causes of SBO
- “SHAVING”
- Stricture
- Hernia
- Adhesions
- Volvulus
- Intussusception/IBD
- Neoplasia
- Gallstone Ileus
References
- Polat C, Aktepe F, Turel S, Yazicioglu B, Ozkececi T, Arikan Y. A giant mesenteric fibromatosis case presenting with mechanical intestinal obstruction and successfully resected with partial duodeno-jejunectomy and right hemicolectomy. Clinics (Sao Paulo). 2010;65(1):110-3. (License: CC BY-4.0)