Anorectal: Abscess & Fistula
Anorectal/Perirectal Abscess
Basics
- Abscess of the Anorectal Region
- Most Common Origin: Anal Glands
- 4-31% Will Recur
- 33-50% Will Develop Fistula-In-Ano
Causes
- Cryptoglandular Disease – Most Common
- Anal Glands/Crypts of Morgagni at the Dentate Line are Blocked Causing Infection
- Inflammatory Bowel Disease – Second Most Common
- Iatrogenic Surgery
- Trauma
- Radiation
- Diverticulitis
- Anal Fissure
- Foreign Body
- Malignancy
- Osteomyelitis
- Infection
Classification
- Perianal: Around Anus Below the Sphincter Complex
- Near Anal Verge
- Ischiorectal: Within Fat of Ischiorectal Fossa
- Tender Away from Anal Verge
- Less Tender on DRE
- Subtypes:
- Postanal Space: Posterior Between the Levators and EAS
- Superficial – Superficial to the Anococcygeal Ligament
- Deep – Deep to the Anococcygeal Ligament
- Often Missed on Drainage – Requires Penetration of the Anococcygeal Ligament
- Horseshoe Abscess: Wraps Around Bilaterally
- Postanal Space: Posterior Between the Levators and EAS
- Intersphincteric: Between Internal and External Sphincter
- Few External Findings
- Significant Tenderness on DRE
- Submucosal: Just Beneath Mucosa Above the Dentate Line
- Supralevator: Above Levator Ani
- Few External Findings
- Need CT to Evaluate
Symptoms
- Anal Pain – Most Common Sx
- Independent from Defecation (Differs from Fissure)
- Fever
- Swelling
Diagnosis
- Classic History and Physical Exam Often Sufficient
- May Require Exam Under Anesthesia (EUA) if Pain Preventing Examination
- Consider CT for Associated Abdominal Sx or Suspicion of Supralevator Source
Treatment
- Primary Tx: Drainage
- Perianal/Ischiorectal: Incision and Drainage (I&D)
- Horseshoe Abscess: Hanley Procedure
- Intersphincteric: Transanal Drainage (Divide IAS)
- Continence Typically Preserved – EAS Not Compromised
- Supralevator: Drain the Source
- Intraabdominal Source: Transabdominal Surgery or Percutaneous Drainage
- Intersphincteric Fistula: Transanal Drainage (Divide IAS)
- Transsphincteric/Ischiorectal Source Through Levators: Ischiorectal I&D
- *See Anorectal: Abscess & Fistula Procedures
- Perianal/Ischiorectal: Incision and Drainage (I&D)
- Antibiotics:
- Most Do Not Require ABX
- Indications:
- Significant Cellulitis
- Diabetes
- Immunosuppression
- Prosthetic Heart Valves
- Systemic Sepsis
- In Profoundly Neutropenic Patients: Consider ABX without I&D
- Do Not Mount Enough of an Immune Response for Suppuration – No Fluctuance to Target for Drainage
- Consider Drainage if Abscess Develops when Neutrophils Rise
- Sepsis or Overt Fluctuance Require Drainage or Debridement
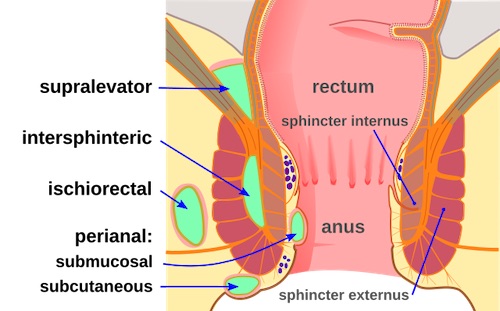
Anorectal Abscess Classification 1
Horseshoe Abscess
Fistula-In-Ano
Basics
- Most Common Cause: Cryptoglandular Disease
- Infection Causes Abscess Leading to Fistula
- External Opening Usually Obvious, Internal More Difficult to Identify
- Goodsall’s Rule
- Anterior Fistulas: Tract Radially to Nearest Crypt
- Straight Path
- Posterior Fistulas: Tract toward Posterior Midline
- Curved Path
- Anterior Fistulas: Tract Radially to Nearest Crypt
Classification
- Route
- Superficial/Subcutaneous: Does Not Involve the Sphincter Complex
- Intersphincteric: Remains in the Intersphincteric Space
- Transsphincteric: Passes Directly Through the EAS
- Suprasphincteric: Extends Proximally in the Intersphincteric Space & Then Extends Through the Levators into the Ischiorectal Fossa
- Extrasphincteric: Tract Extends from the Ischiorectal Fossa Through the Levators into the Rectal Wall
- Complexity
- Simple: No Complex Features
- Superficial/Subcutaneous
- Intersphincteric
- Low Transsphincteric (< 30% of Sphincter Length)
- Single Fistula
- Complex:
- High Transsphincteric Fistula (> 30% of Sphincter Length)
- Suprasphincteric
- Extrasphincteric
- High Blind Tracts
- Multiple Fistulas
- Simple: No Complex Features
Presentation
- Drainage from External Opening – Mucoid, Bloody, Purulent or Feculent
- Recurrent Abscess
- Intermittent Anal Pain
- Anal Pruritis
- Anal Bleeding
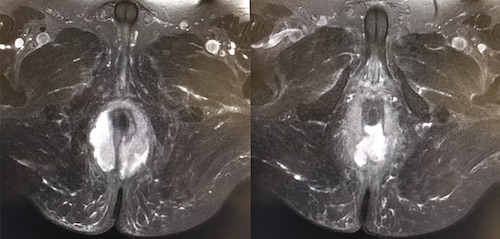
Diagnosis
- Primarily Based on History & Physical Exam
- Simple Fistulas Require No Further Imaging
- Complex Fistulas May Require Imaging to Guide Treatment
- MRI or EUS are Preferred
- Can Determine Presence/Course of Fistulous Tract, Localize Internal Opening, & Delineate Any Extensions
- Imaging-Guided Surgery May Decrease Recurrence Rates for Complex Fistula
Treatment
- Initial Management:
- Simple: Fistulotomy
- Complex: Seton
- Consider Preoperative Transanal US or MRI to Define the Tract
- Staged Procedure Once Tract is Matured (Simple, Narrow and Without Abscess)
- Liberal Use of Setons in Setting of Crohn’s Disease
- Other Options (Generally Used After Setons Fail):
- LIFT Procedure (Ligation of Internal Fistula Tract)
- Rectal Advancement Flap
- Fibrin Glue – Low Success, Generally Abandoned
- Collagen Plug – Low Success, Generally Abandoned
- *See Anorectal: Abscess & Fistula Procedures
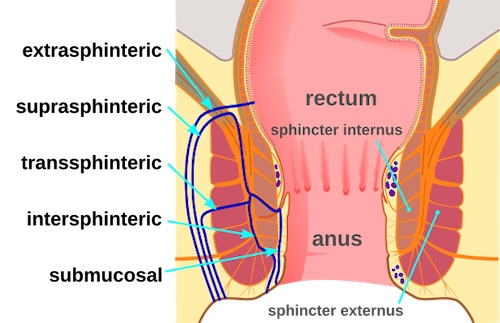
Anorectal Fistula Classification 1
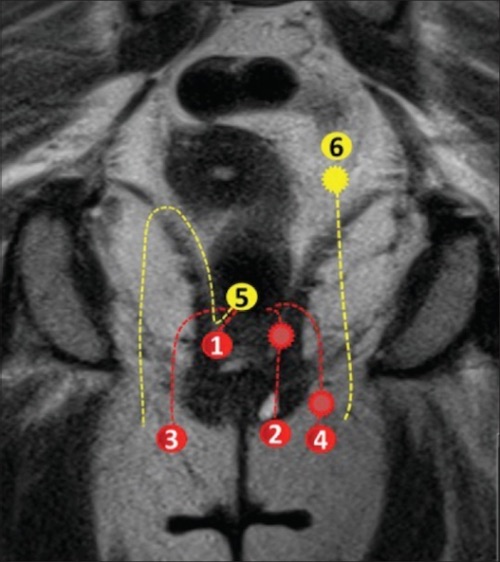
Anorectal Fistula Class by MRI: (1/2) Intersphincteric, (3/4) Transsphincteric, (5) Suprasphincteric, (6) Extrasphincteric 2

Seton 3
References
- Mcort NGHH. Wikimedia Commons. (License: CC BY-SA-4.0)
- Ram R, Sarver D, Pandey T, Guidry CL, Jambhekar KR. Magnetic resonance enterography: A stepwise interpretation approach and role of imaging in management of adult Crohn’s disease. Indian J Radiol Imaging. 2016 Apr-Jun;26(2):173-84. (License: CC BY-NC-SA-3.0)
- Tanner NC, Maw A. A novel technique for negotiation of a complex fistula-in-ano using a flexible ureteral catheter. Ann R Coll Surg Engl. 2014 Jan;96(1):80. (License: CC BY-3.0)