Biliary Tract: Cholecystectomy
Laparoscopic Cholecystectomy
Basics
- Laparoscopic Removal of the Gallbladder
Procedure
- Access Abdomen – x4 Trocars (Periumbilical & x3 Subcostal)
- Expose Gallbladder
- Position Reverse Trendelenburg & Left Side Down
- Retract Fundus Cephalad
- Retract Body Laterally
- *If Difficult to Grab – Consider Decompression by Needle-Aspiration
- Expose the Critical View of Safety
- Divide Cystic Duct & Cystic Artery
- Two Clips Away from the Gallbladder & One Clip Near the Gallbladder
- *Terms Proximal & Distal to the Gallbladder are Generally Discouraged Due to Variability in Meaning
- Dissect Gallbladder from Liver Bed & Remove
- Ensure Hemostasis
- Close Incision Sites
Considerations
- Critical View of Safety – SAGES Safe Cholecystectomy Program
- Only Two Structures Entering Gallbladder (Cystic Artery/Duct)
- Triangle of Calot Cleared of All Fat & Fibrous Tissue
- Lower Third of Gallbladder Separated from Liver
- Encouraged Liberal Use of Intraoperative Cholangiography (IOC)
- Especially in Difficult Cases with Unclear Anatomy
- Routine Use Unnecessary
- If Approaching a Zone of Significant Risk – Finish by a Safe Method:
- Conversion to Open
- Subtotal Cholecystectomy After Removal of All Stones
- Cholecystostomy Tube
- Low Threshold for Calling in Help of Other Experienced Surgeons
Intraoperative Cholangiogram (IOC) & Bile Duct Exploration
Laparoscopic Complications
- Retained Stone
- Stone Retained in Common Bile Duct
- If Intraoperative Concern: Leave T-Tube
- Wait 4-6 Weeks for Tract to Mature Before Instrumentation/Cholangiogram
- If CBD Stone Still Present: Extract Through T-Tube
- Maybe ERCP
- Best Predictor: Persistent High Total Bilirubin
- Spilled Stone
- Stone Spilled into the Peritoneal Cavity
- Can Cause Abscess
- Tx: Laparoscopic Drainage & Stone Removal
- Percutaneous Drain Will Recur
- Biliary Injury (0.26-0.60%)
- The Most Feared & Morbid Complication of Cholecystectomy
- *See Biliary Tract: Biliary Injury
- Bleeding (0.11-1.97%)
- Abscess (0.14-0.30%)
- Bowel Injury (0.14-0.35%)
Conversion to Open Procedure
- Rate of Conversion: Generally Reported as 5-10%
- *Modern Rates Lower and Decreasing
- Risks for Conversion: Elderly, Emergency Status, Male, Low Albumin & Previous Abdominal Surgery
- Modern Surgeons are Generally More Comfortable with Laparoscopic Approaches with Conversion Often Providing Less Benefit
- All Surgeons, However, Should Be Comfortable Opening if Necessary
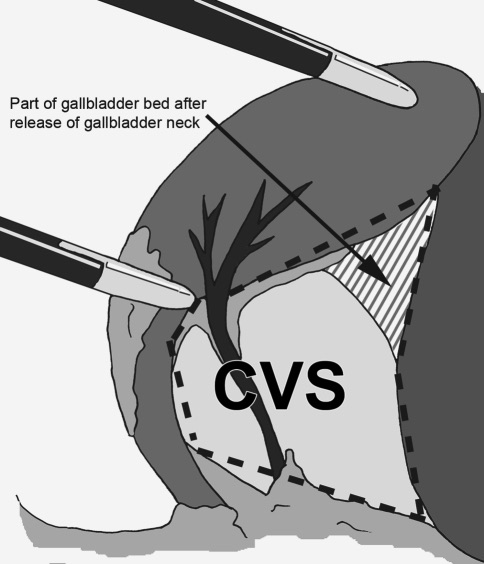
Critical View of Safety 1
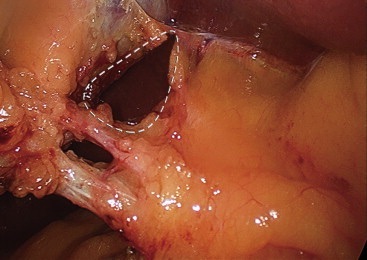
Critical View of Safety 2
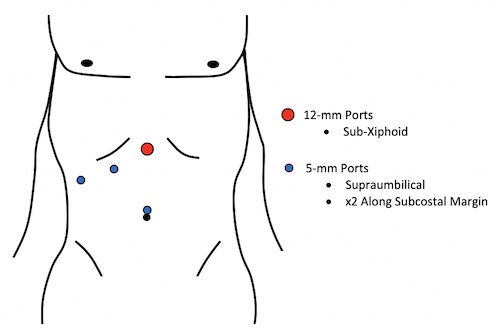
Laparoscopic Port Placement
Open Cholecystectomy
Basics
- Open Removal of the Gallbladder
Indications
- Absolute:
- Unable to Safely Complete Laparoscopic Cholecystectomy
- Unable to Tolerate Pneumoperitoneum
- Hemodynamically Unstable
- Refractory Coagulopathy
- Strong Suspicion of Gallbladder Cancer
- Relative:
- Prior Abdominal Surgery with Significant Adhesions
- History of Cholecystoenteric Fistula
- Cirrhosis
Procedure
- Right Subcostal Incision (Connect Laparoscopic Incisions if Converted)
- “Bottom-Up” Approach
- Starting at Infundibulum
- First Divide Cystic Duct, Then Free from Liver Bed
- Similar Approach as Laparoscopic
- “Top-Down” Approach (Most Commonly Preferred)
- Starting at Fundus
- First Free from Liver Bed, Then Divide Cystic Duct
- Minimize Chance of Duct Injury
Complications
- Compared to Laparoscopic: Higher Mortality & Infection
- Bile Leak – Rare
References
- Wauben LS, Goossens RH, van Eijk DJ, Lange JF. Evaluation of protocol uniformity concerning laparoscopic cholecystectomy in the Netherlands. World J Surg. 2008 Apr;32(4):613-20. (License: CC BY-NC-2.0)
- Dziodzio T, Weiss S, Sucher R, Pratschke J, Biebl M. A ‘critical view’ on a classical pitfall in laparoscopic cholecystectomy! Int J Surg Case Rep. 2014;5(12):1218-21. (License: CC BY-NC-ND-3.0)