Esophagus: Injury & Perforation
Caustic Injury
Basics
- Most Common in Peds After Drinking Household Products
- Type of Necrosis:
- Alkali: Liquefaction Necrosis
- Rapid Extension (Worse)
- Acid: Coagulation Necrosis
- Cause Pain on Contact So Injury is Typically Limited
- Pass Quickly into Stomach with Less Esophageal Injury
- Alkali: Liquefaction Necrosis
- Complications:
- Bleeding
- Fistula
- Stricture – Most Common Late Complication (70%)
- Squamous Cell Carcinoma
Classifications
- Zargar Classification on Endoscopy
- Grade 0: Normal Mucosa
- Grade I: Edema/Erythema
- Grade II: Mucosal/Submucosal Ulceration
- IIa – Hemorrhage, Erosions or Superficial Blisters
- IIb – Circumferential Lesions
- Grade III: Transmural Ulceration with Necrosis
- IIIa – Focal Ulceration
- IIIb – Extensive Ulceration
- Grade IV: Perforation
- Severity Grading
- Low-Grade Injury: Grade 1-2A
- High-Grade Injury: Grade 2B-3
- Pathologic Classification
- Primary (First-Degree): Superficial Mucosa – Hyperemia
- Secondary (Second-Degree): Mucosa/Submucosa – Ulcer & Exudate
- Tertiary (Third-Degree): Transmural – Deep Ulcer & Narrowing
Evaluation
- Evaluation: EGD
- Do Not Pass an Area of Circumferential Injury
Treatment
- Asymptomatic & Low-Volume Ingestion: Discharge
- Symptomatic or High-Volume Ingestion: Conservative Management
- ABX if Suspect Perforation
- Indications for Emergent Surgery:
- Mediastinitis
- Peritonitis
- Transmural Necrosis
- Perforation
- Avoid:
- Nasogastric/Orogastric Tube
- Emetics or Forced Emesis – Re-Exposes Esophagus to Caustic Injury
- Neutralizing Agents – Damage is Typically Immediate
- Corticosteroids
- Follow Up with Screening Endoscopy 10-20 Years Later
Mallory-Weiss & Boerhaave’s Syndrome
Mallory-Weiss Tear/Syndrome
- Partial-Thickness Tear at the GE Junction from Forceful Emesis/Cough
- Linear Laceration of the Mucosa
- Tears Occur Just Below the GE Junction
- More Common in Alcoholics (40-80%)
- Most Common Site: Lesser Curvature Just Below the GE Junction
- Average Length 2-4 cm
- Presentation: Upper GI Bleeding, Pain & Hematemesis
- Tx:
- No Bleeding: Observation
- Bleeding: EGD
- If Fails: Repeat EGD
- If Fails Again: Angioembolization or Gastrostomy & Oversew Vessel
Boerhaave’s Syndrome (Effort Rupture of the Esophagus)
- Esophageal Perforation from Sudden Pressure
- Sudden Increase in Intraesophageal Pressure with Negative Intrathoracic Pressure
- Causes: Vomiting or Severe Straining
- Most Common Site: Left Posterolateral Wall Just Above GE Junction (Around T8)
- Presentation: Retrosternal Chest Pain, Crepitus to Palpation, Pleural Effusion, Odynophagia, Dyspnea, Fever or Epigastric Pains
- Hamann’s Sign: Mediastinal Crunch on Auscultation Synchronous with Heartbeat
- From Pneumomediastinum or Pneumopericardium
- Associated with Tracheobronchial Injury or Boerhaave’s Syndrome
- *Different from Homan’s Sign for DVT’s
- Hamann’s Sign: Mediastinal Crunch on Auscultation Synchronous with Heartbeat
- Dx: Water-Soluble (Gastrografin) Esophagram
- Use Barium if Negative
- Tx: Similar to General Esophagus Perforation
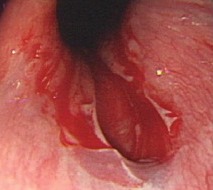
Mallory-Weiss Tear 1
Perforation
Causes
- Iatrogenic (Endoscopy or Nasogastric Tube) – Most Common Cause
- Boerhaave’s Syndrome – Most Common Non-Iatrogenic Cause
- Trauma
- Foreign Body
- Caustic Injury
- Cancer
- Severe Infection
Location
- Most Common Site: Distal Posterolateral Esophagus 2-3 cm Above LES
- Most Common Iatrogenic Site: Cervical Esophagus (Cricopharyngeus Muscle)
Presentation
- Severe Burning Chest Pain
- Epigastric Pain
- Dysphagia
- Odynophagia
- Dysphonia
- Tachycardia
- Fever
- Crepitus
- Pleural Friction Rubs
Diagnosis
- Diagnosis: Gastrografin (Water-Soluble Contrast) Esophagram (“Upper GI”)
- Consider Dilute-Barium if Concerned for Aspiration
- Contrast Agents:
- Barium:Cause Severe Inflammatory Mediastinitis (Should Not Be Used if Concerned for Perforation)
- Generally Provides a Higher Quality Image
- Gastrografin:Causes Severe Pneumonitis (Should Not Be Used if Concerned for Aspiration)
- Barium:Cause Severe Inflammatory Mediastinitis (Should Not Be Used if Concerned for Perforation)
- If Negative but High Suspicion: Repeat Esophagram with Dilute Barium
Treatment
- Initial Management: NPO & ABX (Broad Spectrum & Fungal Coverage)
- May Consider Conservative Managements if Small & Contained or Under 24 Hours
- Persistent Leaks Require Repair
- Primary Tx: Primary Repair Esophageal Stent (Use Evolving)
- Primary Repair
- First Extend Myotomy – To See Full Length of Mucosal Injury
- Debride Devitalized Tissue & Evacuate All Infected Material
- Close in Two Layers: Inner Absorbable, Outer Permanent
- Buttress to Strengthen & Enhance Healing Given no Serosal Layer
- Neck: Strap Muscles or SCM
- Thoracic: Intercostals or Pleural (Less Effective)
- Abdomen: Stomach or Diaphragm
- Leave Wide Drainage
- Esophageal Stent
- Consider if Perforation Contained in Patients That May Not Tolerate Surgery
- Indications Evolving
- Primary Repair
- Diversion:
- Options:
- Neck: Cervical Esophagostomy (Spit Fistula)
- Thoracic: T-Tube (Creates a Controlled Fistula)
- *Consider Gastrostomy Tube for Nutrition
- Indications:
- Unstable
- Extensive Contamination
- Options:
- Special Situations:
- If from Cancer: Esophagectomy
- If from EGD for Achalasia: Also Preform Contralateral Myotomy to Address Underlying Pathology
- If from Trauma: *See Trauma: Esophagus Trauma
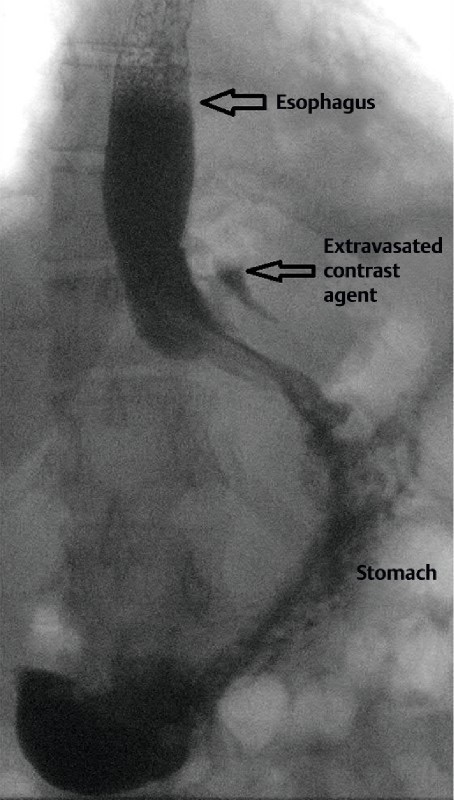
Perforation on Esophagram 2
References
- Na S, Ahn JY, Jung KW, Lee JH, Kim DH, Choi KD, Song HJ, Lee GH, Jung HY, Han S. Risk Factors for an Iatrogenic Mallory-Weiss Tear Requiring Bleeding Control during a Screening Upper Endoscopy. Gastroenterol Res Pract. 2017;2017:5454791. (License: CC BY-4.0)
- Dickinson KJ, Buttar N, Wong Kee Song LM, Gostout CJ, Cassivi SD, Allen MS, Nichols FC, Shen KR, Wigle DA, Blackmon SH. Utility of endoscopic therapy in the management of Boerhaave syndrome. Endosc Int Open. 2016 Nov;4(11):E1146-E1150. (License: CC BY-NC-ND-4.0)