Surgical Critical Care: Hemodynamic Monitoring
Arterial Blood Pressure Monitor (Arterial Line/A-Line)
Indications
- Intraarterial Catheter Used for Continuous Blood Pressure Monitoring
- Other Possible Indications:
- Frequent Blood Sampling
- Arterial Drug Administration
- Use of an Intra-Aortic Balloon Pump (IABP)
Site Selection
- Sites:
- Radial Artery – Generally the Preferred Site
- Central Arteries (Axillary or Femoral)
- Brachial Artery – Worst Choice
- Dorsalis Pedis – Generally Only Used in Children
- Allen Test
- Occlude Radial & Ulnar Arteries, Clench Hand 10x, Release Ulnar Artery
- Positive if Capillary Refill < 6 Seconds
- Indicates Adequate Contralateral Flow
- Poor Accuracy
Radial Artery Placement
- Position: Use a Flexible Board or Rolled Towel to Stabilize the Wrist in Dorsiflexion
- Placed Using Seldinger Technique
- Ultrasound Guidance Should be Utilized if Available
- Benefits:
- Increased First-Pass Success
- Decreased Complication Rate
- Decreased Failure Rate
- Benefits:
Arterial Waveform Analysis
- Arterial Waveform:
- Systolic Upstroke – Systolic Ventricular Ejection
- Systolic Decline – Beginning of Decline Before Diastole
- Dicrotic Notch – Closure of Aortic Valve (Start of Diastole)
- Diastolic Runoff – Decline During Diastole
- System Dampening:
- Over-Dampened System:
- Waveform Appears Flattened with a Small Amplitude & Loss of Dicrotic Notch
- Pressure Changes:
- Decreased Systolic Blood Pressure
- Increased Diastolic Blood Pressure
- Decreased Pulse Pressure
- Causes:
- Air Bubbles in the Tubing
- Arterial Thrombus
- Tube Kinging
- Under-Dampened System:
- Waveform Appears Saltatory & Abrupt with Exaggerated Dicrotic Notch
- Pressure Changes:
- Increased Systolic Blood Pressure
- Decreased Diastolic Blood Pressure
- Increased Pulse Pressure
- Causes:
- Excessively Long Tubing Length
- Multiple Stopcocks
- Over-Dampened System:
- Most Reliable Measure: Mean Arterial Pressure (MAP)
- MAP is Generally Preserved Regardless of Systolic/Diastolic Blood Pressures
- Systolic Blood Pressure is Greater in Peripheral Vessels than in the Aorta
- Due to Smaller Diameter
Complications
- Infection
- Most Common Source: Skin Colonization
- Most Common Organism: S. epidermidis
- Highest Risk Site: Femoral Artery
- Thrombus
- Risk Factors:
- Duration of Use
- Length & Size of Catheter
- Hypercoagulable States
- Clinically Significant Ischemia is Rare (< 1%) – Generally Not a Serious Complication
- Risk Factors:
- Vasospasm
- Distal Ischemia
- Highest Risk Site: Brachial Artery
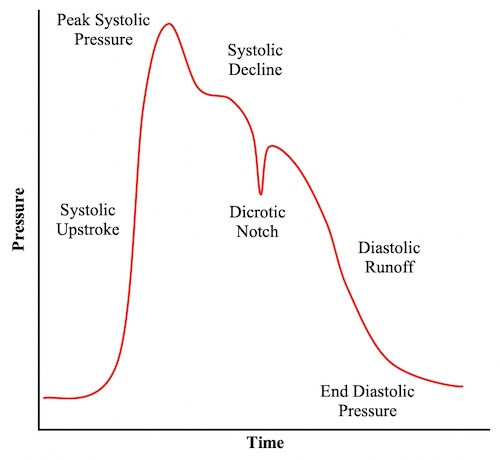
Arterial Waveform
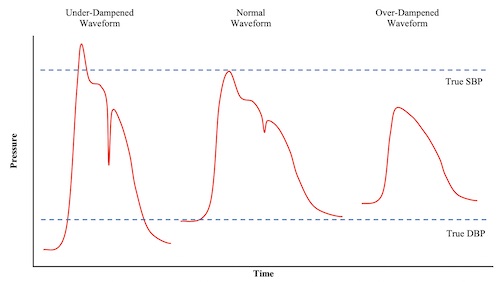
Arterial Waveform Dampening
Pulmonary Artery (Swan-Ganz) Catheter
Basics
- Invasive Catheter Placed into the Pulmonary Artery to Allow Direct Hemodynamic Monitoring
- Catheter Contains 4 Lumens & Thermistor
- White/Clear: Proximal Port (31 cm) – Used for Infusion
- Blue: Distal Right Atrial Lumen (30 cm) – Measures CVP & RA Pressure
- Yellow: Pulmonary Artery Lumen – Measures Pulmonary Artery Pressure & Can Draw Blood for Mixed Venous Oxygen
- Red: Balloon Port
- Thermistor (Red/White Connector) – Measures Cardiac Output by Thermodilution
- Use:
- Can Help in Determining Etiology of Shock & Guide Treatment
- There is No Improvement in Mortality – Therefore it Has Generally Fallen Out of Use
Indications
- Continuous Cardiac Output Monitoring
- Distinguishing Etiology of Shock
- Assessment of Volume Status
- Evaluation of Pulmonary Hypertension
- Evaluation of Pericardial Illnesses
Contraindications
- Absolute Contraindications:
- Presence of a Right Ventricular Assist Device
- Infection at Insertion Site
- Insertion During Cardiopulmonary Bypass
- Relative Contraindications:
- Left Bundle Branch Block (Can Induce RBBB Causing Complete Heart Block)
- Pneumonectomy
- Pacemaker or Defibrillator
- Right-Sided Mechanical Valve
- Right-Sided Endocarditis, Tumors or Masses – Can Cause Embolization (Some Consider an Absolute Contraindication)
- Severe Coagulopathy or Thrombocytopenia
Placement
- Done at Bedside or Under Fluoroscopy (Most Common)
- Insertion Site is Similar to CVC (Right IJ Generally Preferred)
- Confirm Appropriate Position on CXR: West Zone III (Lower Lung Has Less Respiratory Influence)
- Waveforms:
- Right Atrium:
- A Wave (Atrial Contraction) with X Descent
- May Have a Small C Wave (Tricuspid Closure) During X Descent
- V Wave (Ventricular Contraction) with Y Descent
- A Wave (Atrial Contraction) with X Descent
- Right Ventricle: Sharp Systolic Rise/Fall with QRS & Gradual Increase Between
- Pulmonary Artery: Primary Systolic Wave Followed by Gradual Decline with Dicrotic Notch
- Similar to Arterial-Line Waveform
- Pulmonary Artery Wedge Pressure: Similar to Right Atrium but at Higher Pressure
- No C Wave (Tricuspid Closure) During X Descent
- Right Atrium:
Measures
- Measure At: End-Expiration (Lowest Intrathoracic Pressure)
- Measured Values:
- Cardiac Output/Cardiac Index (CO/CI)
- Central Venous Pressure (CVP)
- Pulmonary Artery Wedge Pressure (PAWP)
- Pulmonary Artery Pressure (PAP)
- Mixed Venous Oxygen Saturation (SvO2)
- Temperature
- Calculated Values:
- Stroke Volume (SV)
- Systemic Vascular Resistance (SVR)
- Pulmonary Vascular Resistance (PVR)
Hemodynamic Changes & Shock Differentiation
Complications
- Same Complications as Central Venous Catheters
- Pulmonary Artery Rupture
- Risk: 0.2%
- 30-70% Mortality
- Presentation: Massive Hemoptysis
- Pseudoaneurysm May Form if Initial Injury is Self-Limiting
- Treatment: Leave Balloon Inflated (Tamponade) & Emergent Angiography
- If Fails: Lobectomy
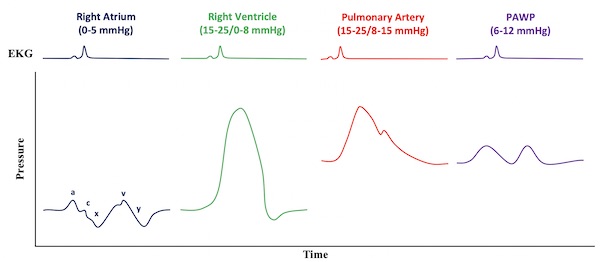
PAC Waveforms
FloTrac/Vigileo
Basics
- Allows for Continuous Minimally Invasive Hemodynamic Monitoring
- Analyzes Arterial Pressure Waveform to Calculate Stroke Volume & Cardiac Output
- Minimally Invasive
- Attaches to an Arterial Line
- Allows Avoidance of Invasive Pulmonary Artery Catheters
- Components:
- FloTrac – Sensor that Connects to the Arterial Line
- Vigileo – Monitor
Measures
- Mean Arterial Pressure (MAP)
- Stroke Volume (SV)
- Cardiac Output/Cardiac Index (CO/CI)
- Stroke Volume Variation (SVV)
- Systemic Vascular Resistance (SVR)
Use
- Generally Accurate in Stable Patients
- SVV if Often Used in Determining Fluid Responsiveness
- *See Surgical Critical Care: Shock
- Accurately Measured Only if Mechanically Ventilated & In Normal Sinus Rhythm
- Accuracy is Controversial for Patients with Low SVR
- Includes: Septic Shock, Hepatic Cirrhosis, Aortic Regurgitation or IABP Counter-Pulsion
Bioreactance/Bioimpedance Analysis (Cheetah NICOM)
Basics
- Allows for Continuous Noninvasive Hemodynamic Monitoring
- Analyzes the “Phase Shifts” When Alternating Current Through the Thorax
- Accurately Measures the Stroke Volume & Heart Rate to Calculate the Cardiac Output
- Noninvasive
- Uses Four External Sensors Over the Thorax
- Allows Avoidance of Invasive Pulmonary Artery Catheters
Measures
- Heart Rate (HR) – Directly Measured
- Stroke Volume (SV) – Calculated Based on Flow (dX/dt) & Ventricular Ejection Time (VET)
- Age & Body Surface Area (Weight & Height) Affect Signal Propagation & Are to Modify the Calculation
- Cardiac Output (CO) – Calculated from HR & SV
- CO = SV x HR = f(dX/dt,VET,HR,Weight,Height,Age)