Surgical Critical Care: Central Venous Catheter (CVC)
Central Venous Catheter (CVC) Basics
Anatomy Review
- Internal Jugular (IJ) Vein
- Lies Under the Sternocleidomastoid Muscle (SCM)
- Vein Runs Anterior & Lateral to the Carotid Artery
- Subclavian (SC) Vein
- Runs Under Clavicle
- Subclavian Artery & Brachial Plexus Are Deep to the Vein
- Femoral Vein
- Runs Medial to the Femoral Artery
Types
- Non-Tunneled CVC
- Direct Protrusion of Catheter
- Placed at Bedside
- Tunneled CVC
- Passed Under Skin to Separate Site
- Placed by IR or in OR
- *Lower Infection Risk
- Peripherally Inserted Central Catheter (PICC)
- Longer Line Placed Peripherally in an Arm Vein
- Less Invasive & Lower Infection Risk
- Smaller Caliber Lumens
- Often Used if Anticipating Long-Term Need (TPN or ABX)
- Subcutaneous Port
- Completely Tunneled with No Exposed Ports
- Placed Under Anesthesia
- Lower Infection Risk than Tunneled or Non-Tunneled CVC
- Longer Patency – Ideal for Chemotherapy
Choice of Site
- Generally Preferred CVC Route: Right IJ
- Straight Path into the SVC – Low Rate of Catheter Malposition
- Able to Provide Compression for Bleeding Easier than SC Vein
- If Patient Already Has a Pneumothorax/Chest Tube – Strongly Consider Placing Central Line on the Ipsilateral Side (If Placement is Complicated by Pneumothorax it is Already Treated – “Free Shot”)
- Comparison:
- Subclavian
- Lowest DVT Risk
- Lowest Infection Risk
- Highest Mechanical Complication (PTX, etc.) Risk
- Femoral
- Lowest Mechanical Complication (PTX, etc.) Risk
- Subclavian
CVC Flow
- Hagen-Poiseuille Equation
- Flow (Q) = ΔP x πr4 / 8 µL
- P = Pressure, r = Radius, µ = Viscosity, L = Length
- Directly Related to Radius4
- Inversely Related to Length1
- Flow (Q) = ΔP x πr4 / 8 µL
- Increased Flow with Higher Radius (Strongest Factor) & Lower Length
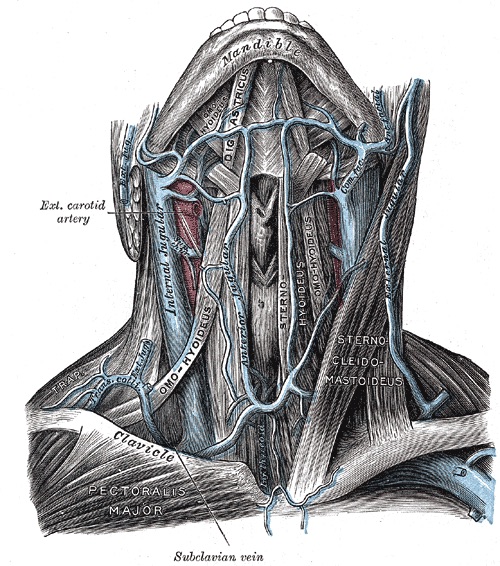
Internal Jugular Vein & Subclavian Vein 1
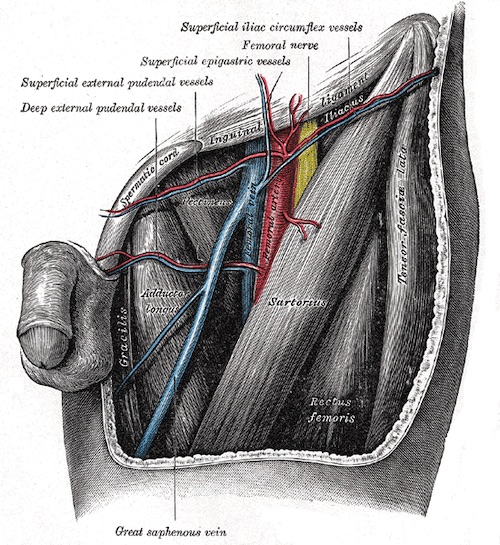
Femoral Vein 1
Placement
Techniques
- Blind Placement – Based Solely on Anatomy without US Guidance
- Ultrasound Guidance Should be Utilized if Available
- Benefits:
- Decreased Complication Rate
- Decreased Failure Rate
- Increased First-Pass Success
- Benefits:
- *Either Method Utilizes a Seldinger Technique
Position/Prep
- Supine or Head-Down 10-20 Degrees
- For Subclavian Vein CVC – Arm Should be Completely Adducted
- Procedure Should be Performed in a Sterile Manner Unless Absolute Unable
Blind Placement
- Internal Jugular (IJ) Vein
- Insertion:
- Anterior Approach: Along the Medial Border of the SCM, 2-3 Fingerbreadths Above the Clavicle
- Central Approach: The Apex of the Bifurcation of the SCM Heads
- Angle: 30-45 Degrees
- Aim: Ipsilateral Nipple
- *Palpate the Carotid Artery During Placement (Vein Should be Lateral to Pulse)
- Insertion:
- Subclavian Vein
- Insert: 2-3 cm Below Midpoint of Clavicle (1-2 cm Lateral of Bend)
- Aim: Just Deep to Suprasternal Notch
- If Clavicle is Hit, Withdraw and March Down
- Femoral Vein
- Insert: 1-2 cm Below Inguinal Ligament & 1 cm Medial to the Femoral Artery Pulse
- Angle: 30-45 Degrees
Seldinger Technique
- Puncture Vein with Hollow Introducer Needle
- Attach Syringe with Gentle Negative Pressure During Advancement
- Dark Non-Pulsatile Blood Confirms Venipuncture (Caution: Arterial Blood in Hypoxic Patients May Also be Dark)
- Pass Guidewire Through the Needle
- Always Maintain Control of the Guidewire During Placement – Should Never Completely Enter the Vein
- Withdraw Needle
- Make Small Skin Incision at the Entry Site
- Pass Dilator Over the Guidewire & Remove the Dilator
- Pass CVC Over the Guidewire
- Withdraw Guidewire
- Suture CVC to Skin & Place Sterile Dressing
- Always Obtain Post-Procedure Chest XR to Confirm Appropriate Positioning & Look for Pneumothorax
Goal Tip Location
- CVC: 1-2 cm Above the Right Atrium-SVC Junction
- Seen as Just Above the Carina on CXR
- Dialysis Catheter: Right Atrium
- Higher Flow Rate
Insertion Length
- Equation Based on Height (cm):
- Right SC: Height/10 – 2 cm
- Right IJ: Height/10
- Left SC: Height/10 + 2 cm
- Left IJ: Height/10 + 4 cm
- General Lengths:
- Right SC: 11-14 cm
- Right IJ: 13-15 cm
- Left SC: 15-17 cm
- Left IJ: 17-18 cm
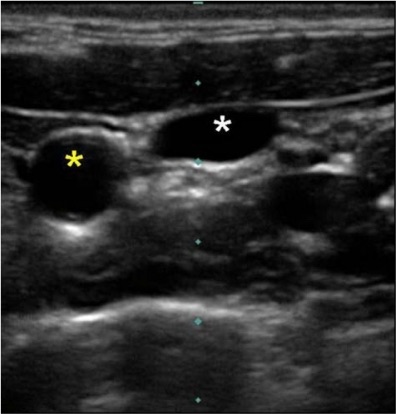
US Guidance Showing Compressibe IJ (White Star) and Noncompressible Carotid (Yellow Star) 2
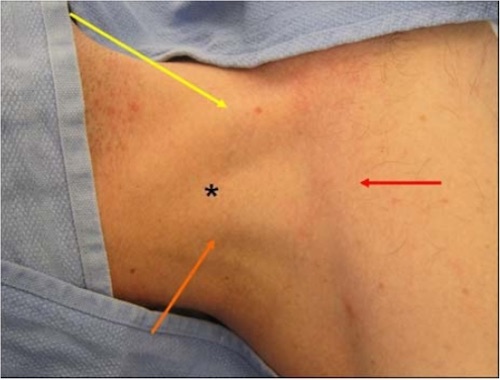
IJ Insertion (Star), SCM Sternal Head (Yellow), SCM Clavicular Head (Orange), Clavicle (Red) 2
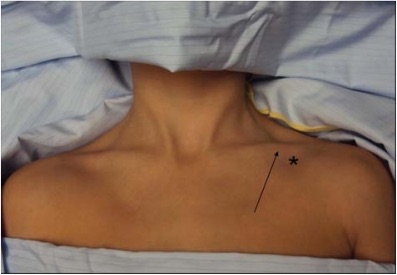
SC Insertion (Star), Bend of Clavicle (Arrow) 2
Complications
Carotid Cannulation (Arterial Injury)
- Can Cause Life-Threatening Hemorrhage
- Reduce Risk by Using Ultrasound-Guidance for Placement
- Diagnosis:
- ABG
- Pressure Transducer Showing Arterial Waveform
- CXR Showing Line to the Left of the Spine
- Treatment:
- Cannulation with Probe Needle Only: Remove & Hold Pressure for 5-10 Minutes
- Cannulation with Dilator or Catheter: Remove in OR
Malposition
- Tip Abutting into the Wall of the Superior Vena Cava
- Risk for SVC Puncture
- Treatment: Retract to the Innominate Vein (Do Not Advance)
- Tip in Right Atrium
- Risk for Atrial Wall Puncture
- Treatment: Retract to the Right-Atrium-SVC Junction
Pneumothorax (PTX)
- Risk: 1-6.6% (Higher Risk in Emergency Setting or if Multiple Needle Passes are Required to Find the Vein)
- *See Trauma: Pulmonary Trauma
Cardiac Tamponade
- From Puncture of the Right Atrium
- *See Trauma: Cardiac Trauma
Thrombosis
- *See Vascular: Deep Venous Thrombosis (DVT)
- Treatment:
- If Catheter Not Needed: Remove & Heparin
- If Catheter Needed: Systemic Heparin or tPA Down the Line
Air Embolism
Central Line-Associated Bloodstream Infection (CLABSI)
- Also Known as Catheter-Related Bloodstream Infection (CRBSI)
- Risk Increases with Duration of Placement (However there is No Indication for Routine Catheter Changing Based on the Number of Days)
- Most Common Source: Skin Colonization
- Most Common Organisms:
- S. epidermidis (Most Common)
- S. aureus (Second Most Common)
- Enterococci
- Candida
- Presentation:
- Inflammation & Purulence at the Catheter Insertion Site
- Fever
- Sepsis (Often Sudden Onset)
- Complications:
- Septic Thrombophlebitis
- Infective Endocarditis
- Treatment: Antibiotics & Catheter Removal
- If Clinically Unable to Remove the Catheter – Consider Exchange Over a Guidewire

CVC in Aorta
References
- Gray H. Anatomy of the Human Body (1918). Public Domain.
- Bannon MP, Heller SF, Rivera M. Anatomic considerations for central venous cannulation. Risk Manag Healthc Policy. 2011;4:27-39. (License: CC BY-NC-3.0)