Endocrine: Hypercortisolism (Cushing Syndrome)
Hypercortisolism (Cushing Syndrome)
Definition
- Excess Cortisol from Exogenous Administration or Endogenous Production
Causes
- Exogenous Steroids (Iatrogenic/Factitious) – #1 Most Common Cause Overall
- Endogenous Causes:
- ACTH-Dependent Causes:
- Cushing Disease/Pituitary ACTH Adenoma (65-70% Most Common Endogenous Cause & #2 Overall)
- Ectopic ACTH Secretion (10-15%)
- Most Common Source: Squamous Cell Lung Cancer
- Ectopic CRH Secretion (< 1%)
- Exogenous ACTH Administration (<1%)
- ACTH-Independent Causes:
- Adrenal Adenoma/Carcinoma (18-20%)
- Adrenal Hyperplasia
- Primary Pigmented Nodular Adrenocortical Disease (< 1%)
- Bilateral Macronodular Adrenal Hyperplasia (< 1%)
- ACTH-Dependent Causes:
Presentation
- Abnormal Glucose Intolerance
- Hypertension
- Weight Gain:
- Central Obesity
- Round “Moon” Face (Fat Accumulation in Cheeks)
- “Buffalo Hump” (Dorsal Fat Pad)
- Skin Changes:
- Purple Striae
- Acne
- Easy Bruising/Ecchymosis
- Hyperpigmentation – If Due to Excess ACTH (Pituitary Adenoma or Ectopic Production)
- ACTH Converted to MSH (Melanocyte Stimulating Hormone)
- Reproductive:
- Menstrual Irregularity
- Decreased Libido
- Hirsutism
- Pain:
- Abdominal Pain
- Headache
- Back Ache
- Musculoskeletal:
- Proximal Muscle Weakness
- Osteoporosis
- Psychologic Changes:
- Lethargy
- Depression
- Anxiety
- Irritability
Diagnosis
- First Exclude Exogenous Steroids Before Starting Testing
- #1 Screen: 24-Hour Urine Cortisol (Best Screening Test)
- Other Screening Tests:
- Low-Dose Dexamethasone Suppression Test
- Late-Night Salivary or Serum Cortisol
- Other Screening Tests:
- #2 Determines ACTH Dependence: Plasma ACTH Level
- Low ACTH (< 5 pg/mL): Indicates ACTH Independence (Adrenal Source)
- High ACTH (> 20 pg/mL): Indicates ACTH Dependence (Extra-Adrenal Source)
- *If Intermediate (5-20 pg/mL): Likely Dependent but Consider CRH Stimulation Test
- #3 Determine ACTH Source if Dependent: High-Dose Dexamethasone Suppression Test
- Cortisol Suppressed: Indicates a Pituitary Tumor
- Cortisol Not Suppressed: Indicates an Ectopic ACTH Source
- *If Indeterminate: Consider Inferior Petrosal Sinus Sampling (IPSS) to Directly Measure Pituitary ACTH Secretion
- Radiographic Localization/Definition:
- Adrenal Source: CT Adrenal Glands
- Pituitary Tumor: Pituitary MRI
- Ectopic ACTH: CT Chest (#1) & CT Abdomen
Treatment
- Exogenous Steroids: Tapered Steroid Withdrawal
- Abrupt Discontinuation Will Cause Adrenal Insufficiency
- Cushing Disease (Pituitary ACTH Adenoma): Transsphenoidal Resection
- If Unresectable: Medical Management or Radiation Therapy
- Ectopic ACTH or CRH Secretion: Resect Primary Tumor
- Options If Unresectable: Medical Management or Bilateral Adrenalectomy
- ACTH-Independent (Adrenal Source): Adrenalectomy
- *See Endocrine: Adrenalectomy
- Extent:
- Adrenal Adenoma: Unilateral Adrenalectomy
- Adrenal Hyperplasia: Bilateral Adrenalectomy
- If Unresectable or Not Surgical Candidate: Medical Management
Specific Treatment Considerations
- Medical Management:
- Adrenal Enzyme Inhibitors (Ketoconazole, Metyrapone or Etomidate)
- Mitotane (Adrenal Enzyme Inhibitor & Adrenal Lytic)
- Surgical Approach:
- Laparoscopic Adrenalectomy is Preferred if Able
- Open (Anterior) Approach if Large > 6-7 cm
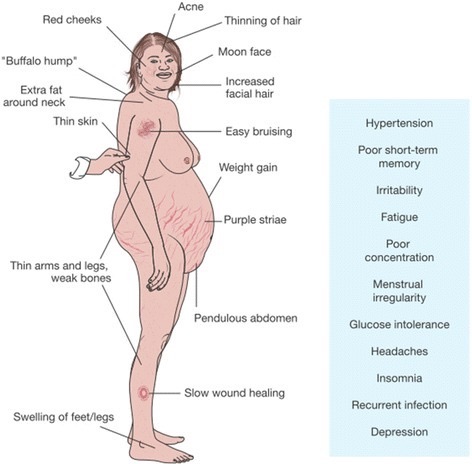
Cushing Syndrome Appearance 1

Moon Face; Before (Left) and After (Right) 2

Buffalo Hump 3

Purple Striae 4
References
- Brue T, Castinetti F. The risks of overlooking the diagnosis of secreting pituitary adenomas. Orphanet J Rare Dis. 2016 Oct 6;11(1):135. (License: CC BY-4.0)
- Celik O, Niyazoglu M, Soylu H, Kadioglu P. Iatrogenic Cushing’s syndrome with inhaled steroid plus antidepressant drugs. Multidiscip Respir Med. 2012 Aug 29;7(1):26. (License: CC BY-2.0)
- Medappil N, Vasu TA. Madelung’s disease: A spot diagnosis. Indian J Plast Surg. 2010 Jul;43(2):227-8. (License: CC BY-2.0)
- Vilallonga R, Zafon C, Fort JM, Mesa J, Armengol M. Past and present in abdominal surgery management for Cushing’s syndrome. SAGE Open Med. 2014 Mar 31;2:2050312114528905. (License: CC BY-NC-3.0)