Pancreas: Pancreatic Neuroendocrine Tumor (PNET)
Pancreatic Neuroendocrine Tumor (PNET)
Definitions
- Pancreatic Neuroendocrine Neoplasia (PNEN) – All Neuroendocrine Neoplasias in the Pancreas
- Previously Known as Islet Cell Tumors
- Pancreatic Neuroendocrine Tumor (PNET) – Well Differentiated
- Pancreatic Neuroendocrine Carcinoma (PNEC) – Poorly Differentiated Histology & High-Proliferative Rate
Non-Functional Endocrine Tumor
- Secrete Substances but Do Not Present with Hormonal Syndromes
- Can Secrete Chromogranin, Pancreatic Polypeptide, Ghrelin, etc.
- Present Later with More Indolent & Protracted Course
- Most Common PNET (50-85%)
- Presentation:
- Abdominal Pain
- Weight Loss
- Anorexia
- Nausea
Insulinoma
- Insulin Secreting Tumor
- Most Common Functional PNET
- Most are Benign (93%)
- Evenly Distributed Throughout Pancreas Mn
- Presentation:
- Symptoms:
- Confusion
- Visual Changes
- Palpitations
- Diaphoresis
- Amnesia
- Whipple’s Triad:
- Fasting Hypoglycemia
- Symptoms of Hypoglycemia
- Relief with Glucose
- Symptoms:
- High C-Peptide – If Low: Consider Exogenous Insulin Administration (Munchausen’s Syndrome)
Glucagonoma
- Glucagon Secreting Tumor
- Most are Malignant (50-80%)
- Most Common in Body & Tail Mn
- Presentation:
- Symptoms:
- Weight Loss (Most Common Presenting Symptom)
- Stomatitis
- Diarrhea
- 4-D’s Syndrome:
- Diabetes (Glucose Intolerance)
- DVT
- Depression
- Dermatitis (NME)
- Necrolytic Migratory Erythema (NME)
- Erythematous Papules of Face, Perineum & Extremities
- Enlarge Over 1-2 Weeks Then Have Central Clearing with Indurated Blisters and Crust
- From Malnutrition & Amino Acid Deficiency
- Treatment: Supplementation (Zinc, Amino Acids & Fatty Acids)
- Resolves with Tumor Resection
- Erythematous Papules of Face, Perineum & Extremities
- Symptoms:
Gastrinoma
Somatostatinoma
- Somatostatin Secreting Tumor
- Most are Malignant (75%)
- Most Common in Head Mn
- Presentation:
- Most Common Symptoms: Abdominal Pain & Weight Loss
- Somatostatinoma Syndrome
- Triad:
- Diabetes
- Cholelithiasis
- Diarrhea/Steatorrhea
- Less Commonly Seen (19% if in Pancreas or 2% if in Duodenum)
- Triad:
VIPoma
- VIP Secreting Tumor
- Most are Malignant (60-80%)
- Most Common in Body & Tail Mn
- Presentation:
- VIPoma Syndrome (WDHA Syndrome/Verner-Morrison Syndrome)
- Profuse Watery Diarrhea (> 700 mL/Day) that Persists with Fasting
- “WDHA”: Watery Diarrhea, Hypokalemia & Achlorhydria (HCl)
- Electrolyte Losses Due to Profound Diarrhea
- Causes Metabolic Acidosis
- VIPoma Syndrome (WDHA Syndrome/Verner-Morrison Syndrome)
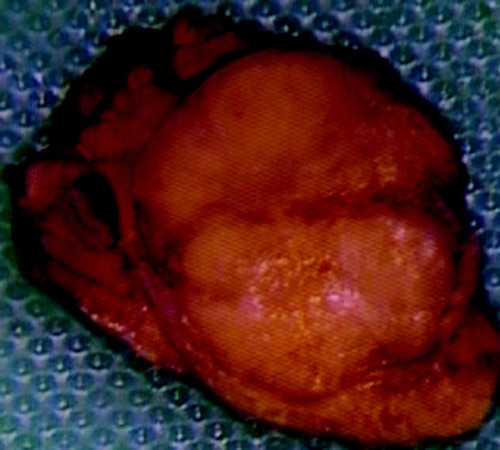
Insulinoma 1
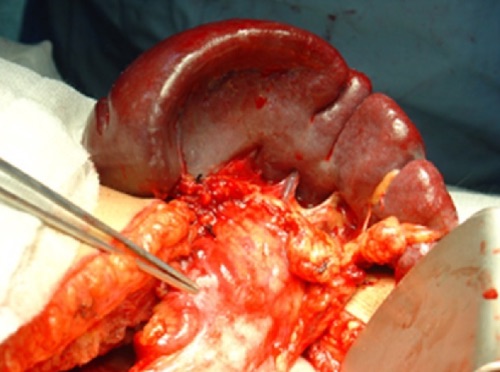
Glucagonoma in Pancreatic Tail 2

Necrolytic Migratory Erythema (NME) 3
PNET – Staging & Variation
TNM Staging – AJCC 8
- TNM
| T | N | M | |
| 1 | < 2 cm | N+ | M1a – Liver
M1b – Extrahepatic M1c – Liver & Extrahepatic |
| 2 | ≥ 2 cm | ||
| 3 | > 4 cm or Invades Duodenum/CBD | ||
| 4 | Invades Adjacent Organs or Large Vessels |
- For T Stage – Multiple Tumors are Designated as T(#) (Example: T3(4))
- If Number or Tumors is Too Numerous or Unavailable – T(m)
- For T Stage – Multiple Tumors are Designated as T(#) (Example: T3(4))
- Stage
| T | N | M | |
| I | T1 | N0 | M0 |
| II | T2-3 | N0 | M0 |
| III | T4 | N0 | M0 |
| Any T | N1 | M0 | |
| IV | Any T | Any N | M1 |
Histologic Grading
- Well-Differentiated
- PNET-G1 (Low-Grade): Ki-67 < 3% or Mitotic Index < 2
- PNET-G2 (Intermediate-Grade): Ki-67 > 3% or Mitotic Index > 2
- PNET-G3 (High-Grade): Ki-67 > 20% or Mitotic Index > 20
- Poorly-Differentiated
- PNEC-G3: Ki-67 > 20% or Mitotic Index > 20
Malignancy
- Most are Malignant
- Insulinoma Mostly Benign
- Gastrinoma 50-60%
- 75% Present as Advanced Disease
- Most Common Site of Mets: Liver
Association with MEN-1
- Most Commonly Spontaneous
- Insulinoma: 6%
- Glucagonoma: 20%
- Gastrinoma: 20-30%
- Most Common PNET in MEN-1 Syndrome
- Somatostatinoma: 35-45%
- Although One of the Least Common Overall
- VIPoma: 5%
Location
- Most Common in Head: Gastrinoma & Somatostatinoma
- Most Common in Body & Tail: Glucagonoma & VIPoma
- Even Distribution: Insulinoma
PNET – Management
Diagnosis
- Insulinoma: High Insulin & Hypoglycemia
- Produce Hypoglycemia By 72-Hour Fast or Mixed-Meal Test
- Rule Out Exogenous Administration:
- C-Peptide Level – Low Values Indicate Exogenous Insulin
- Sulfonylurea Screen & Meglitinide Screen
- Glucagonoma: High Fasting Glucagon (> 500 pg/mL)
- Gastrinoma: Secretin Stimulation Test (Causes Marked Gastrin Increase)
- Somatostatinoma:
- If Somatostatinoma Syndrome Present: High Fasting Somatostatin (> 30 pg/mL)
- If Not Present (Most Common): Specimen Histology Stain Positive for Somatostatin
- VIPoma: High Serum VIP (> 75 pg/mL)
Localization
- Initial: CT or MRI
- If Fails: Somatostatin Receptor Imaging
- Not Used for Insulinomas (Low Somatostatin Receptor Expression)
- Tests:
- Somatostatin (Octreotide) Receptor Scintigraphy (SRS)
- Classically Used
- Functional PET Scans
- Becoming More Prevalent with Higher Sensitivity
- Radiotracer: Ga-68 DOTATATE or Ga-68 DOTATOC
- Somatostatin (Octreotide) Receptor Scintigraphy (SRS)
- If Imaging Fails: EUS
- If EUS Fails: Invasive Testing
- Selective Arterial Stimulation with Hepatic Venous Sampling
- Use: Insulinoma (Calcium Stimulation) or Gastrinoma (Secretin Stimulation)
- Selective Visceral Angiography
- Use: Glucagonoma, Somatostatinoma or VIPoma
- Selective Arterial Stimulation with Hepatic Venous Sampling
- If High Suspicion of Gastrinoma & All Testing Fails: Surgical Exploration
Treatment
- Resectable:
- < 2-3 cm: Enucleate
- Should Be ≥ 2-3 mm From the Main Pancreatic Duct (Reduce Leak Risk)
- *May Consider Observation in Select Patients
- *Enucleation is Controversial for the More Malignant PNETs (VIPoma, Somatostatinoma or Glucagonoma)
- > 2-3 cm, Local Invasion or N+: Resection
- Head/Neck: Pancreaticoduodenectomy
- Body/Tail: Distal Pancreatectomy
- If Malignancy Suspected: Concurrent Splenectomy
- Entire Pancreas: Total Pancreatectomy
- < 2-3 cm: Enucleate
- Unresectable or Mets:
- Resect Mets if Able
- Symptomatic Treatment:
- Insulinoma – Diazoxide (Inhibits Insulin Release)
- If Fails: Octreotide or Everolimus
- Gastrinoma – PPI
- If Fails: Octreotide
- Others – Octreotide
- Insulinoma – Diazoxide (Inhibits Insulin Release)
- If Severe/Enlarging: Chemotherapy
- Classic Regimen: Streptozocin with/without Doxorubicin (Toxic to Beta Cells)
- Newer Regimen: Temozolomide with/without Capecitabine (CAPTEM)
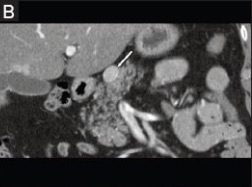
PNET on CT 4
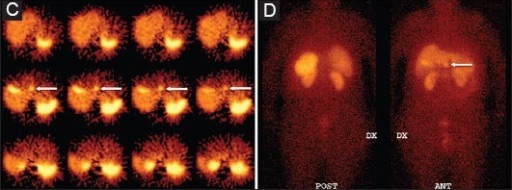
PNET on SRS 4
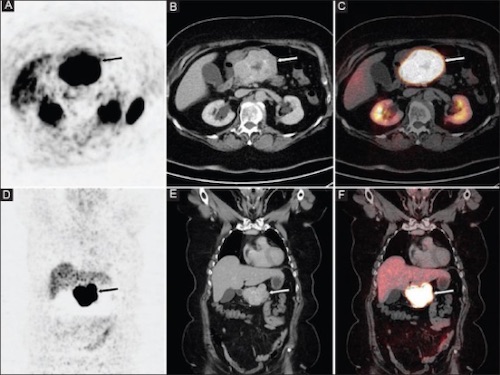
PNET on Functional PET 4

PNET on EUS 4
Pancreatic Neuroendocrine Carcinoma (PNEC)
Basics
- Poorly Differentiated Histology & High-Proliferative Rate
- Almost All are Non-Secretory
- Aggressive – Most Are Metastatic at Time of Presentation
- Sx: Abdominal Pain, Nausea, Fatigue & Weight Loss
Diagnosis
- Requires Bx with Neuroendocrine Markers (Chromogranin & Synaptophysin)
- Imaging: CT, MRI or PET
- Somatostatin Receptor Imaging Usually Not Helpful
Treatment
- Resect if Able
- Chemotherapy for All
- Platinum-Based (Carboplatin or Cisplatin) & Etoposide
Mnemonics
Most Common Site of PNET’s
- #6 – The Number of the Pancreas (Used in Other Mnemonics: Pseudocyst and Chronic Pancreatitis)
- Pancreas Looks Like a #6
- “SIX” Written on Pancreas:
- “S” in Head: gaStrin & SomatoStatin
- “I” Anywhere: Insulin
- “X” in Body/Tail: Glucagon & VIP
#6 – The Number of the Pancreas
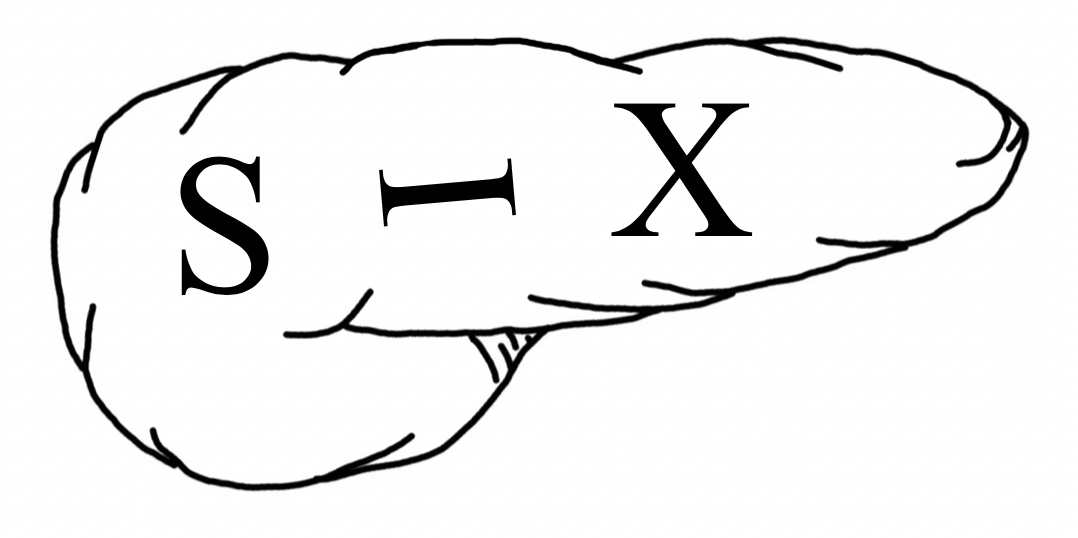
#6 – The Number of the Pancreas
References
- Alabraba E, Bramhall S, O’Sullivan B, Mahon B, Taniere P. Pancreatic insulinoma co-existing with gastric GIST in the absence of neurofibromatosis-1. World J Surg Oncol. 2009 Feb 13;7:18. (License: CC BY-2.0)
- Al-Faouri A, Ajarma K, Alghazawi S, Al-Rawabdeh S, Zayadeen A. Glucagonoma and Glucagonoma Syndrome: A Case Report with Review of Recent Advances in Management. Case Rep Surg. 2016;2016:1484089. (License: CC BY-4.0)
- Pakran J, Riyaz N. Necrolytic migratory ulceration. Indian Dermatol Online J. 2013 Jul;4(3):205-7.(License: CC BY-NC-SA-3.0)
- Kartalis N, Mucelli RM, Sundin A. Recent developments in imaging of pancreatic neuroendocrine tumors. Ann Gastroenterol. 2015 Apr-Jun;28(2):193-202. (License: CC BY-NC-SA-3.0)