Vascular: Peripheral Arterial Disease (PAD)
Peripheral Arterial Disease (PAD)
Basics
- Definition: Narrowed Arteries Causing Decreased Blood Flow to Extremities
- Most Common Cause: Atherosclerosis
Risk Factors
- Tobacco – Strongest Risk Factor
- Diabetes – Second Strongest Risk Factor
- Elderly
- Proximal Aortoiliac Disease Associated with Younger Age
- Hypertension
- Hyperlipidemia
- Renal Disease
- Hyperhomocysteinemia
- Male Sex
Prognosis
- Strong Predictor of Future Cardiovascular Disease (MI or CVA)
- 5-Year Mortality:
- Asymptomatic: 19%
- Symptomatic: 24-30%
- Risk of Future Major Amputation with Claudication: 1% per Year
- 5-Years: < 5%
- 10-Years: 12%
- 7% (4-11%) of Asymptomatic Patient Will Develop Intermittent Claudication After 5-Years
Site of Stenosis
- Generally Divided into 3 Levels:
- Aortoiliac Disease
- Femoropopliteal Disease
- Tibioperoneal Disease
- Most Common Sites:
- Overall in Legs: Hunter’s Canal
- In Smokers: Superficial Femoral Artery
- In DM/CKD: Infrapopliteal Disease
- Least Likely Site: Peroneal Artery – Due to Deep Compartment Location
Medial Calcinosis (Monckeberg Arteriosclerosis)
- Cause: Calcification of Tunica Media
- Seen in DM & ESRD
- Most Common Site: Tibial Vessels
- Vessels are Rigid & Difficult to Compress (Falsely Elevated ABI)
- Spares Digital Vessels (Toe Pressure & Transcutaneous Oximetry More Reliable)
Presentation
- Most Commonly Asymptomatic & Found Incidentally
- Intermittent Claudication (Activity-Induced Pain)
- Site of Occlusion – Level of Symptoms
- Aortoiliac – Buttock, Hip & Thigh
- External Iliac – Thigh
- Femoral – Calf
- Popliteal – Foot
- Infrapopliteal – Often Have No Pain
- Calf Pain is the Most Common Site
- Site of Occlusion – Level of Symptoms
- Ischemic Resting Pain
- Ulceration & Gangrene
- Critical Limb Ischemia
- Muscle Atrophy
- Leriche Syndrome
- Triad: Diminished Femoral Pulse, Buttock Claudication & Impotence
- Indicates Aortoiliac Occlusive Disease
Symptomatic Grouping
- Intermittent Claudication (IC) – Activity-Induced Pain but Not at Rest
- Chronic Limb-Threatening Ischemia (CLTI) – Rest Pain or Tissue Necrosis
- *Previously Called Critical Limb Ischemia (CLI)
- Acute Limb Ischemia (ALI) – *See Vascular: Acute Limb Ischemia
Diagnosis
- Ankle-Brachial Index (ABI)
- Best Initial Screening Test
- ABI = Ankle / Brachial Blood Pressure
- Ankle: Highest DP or PT on That Side
- Brachial: Highest on Either Side Used for Both Legs
- Values:
- 0.9-1.2 – Normal (When Supine Arm May Be 20% Higher Than Ankle)
- < 0.9 – Diagnostic of PAD
- < 0.7 – Often See Claudication
- < 0.4 – Often See Rest Pain
- < 0.3-0.4 – Often See Ulcers & Gangrene
- Not Reliable in DM or ESRD – Calcified Vessels Give False Elevation
- If Initial ABI is Normal Despite Claudication Symptoms – Consider Repeat ABI After Exercise
- Doppler US
- Useful Bedside Exam in Evaluation but Need More for Diagnosis
- Waveforms:
- Normal: Triphasic
- Systole – Rapid Antegrade Flow
- Early Diastole – Transient Retrograde Flow
- Late Diastole – Slow Antegrade Flow
- Abnormal: Biphasic, Monophasic or None
- Waveform Flattens & Early Diastolic Retrograde Flow is Lost
- Normal: Triphasic
- Arterial Duplex US
- Good for Initial Work-Up
- “Duplex” – Pulsed Doppler System (Velocity) & Real-Time B Mode US (Image)
- CTA
- Typically the Diagnostic Modality of Choice
- Angiography
- Gold Standard but More Invasive
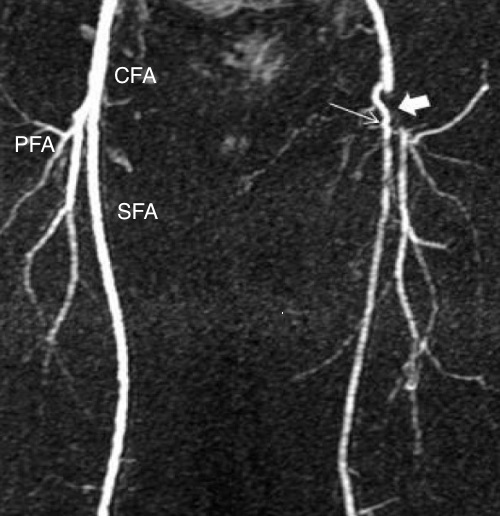
MRA Demonstrating CFA Stenosis 1
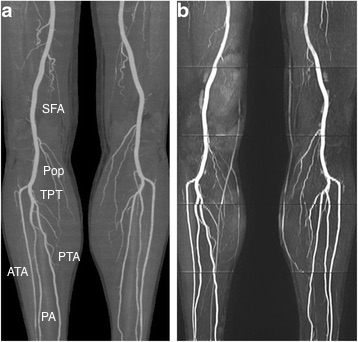
Normal Distal Angiogram 2
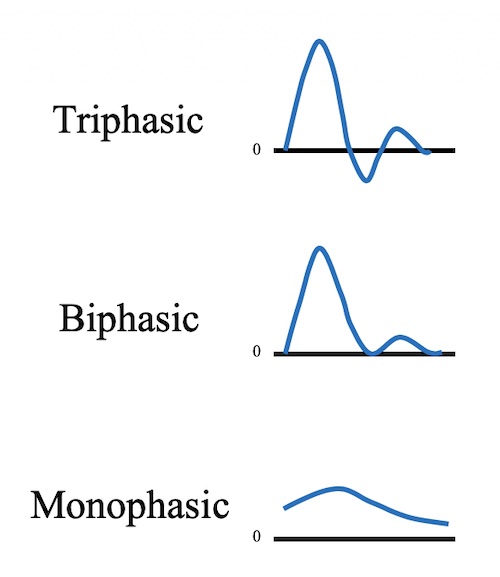
Doppler Waveforms
Peripheral Arterial Disease (PAD) – Classification
Fontaine Stages
- Stage I: Asymptomatic
- Stage II: Claudication
- IIa: Mild (At Distance > 200 m)
- IIb: Moderate-Severe (At Distance < 200 m)
- Stage III: Ischemic Rest Pain
- Stage IV: Ulceration or Gangrene
Rutherford Grades/Categories for Chronic Limb Ischemia
| Grade | Category | Clinical Description | Objective Criteria |
| 0 | 0 | Asymptomatic | Normal Treadmill or Reactive Hyperemia Test |
| I | 1 | Mild Claudication | Completes Treadmill Exercise
AP > 50 mmHg After Exercise but ≥ 20 mmHg Under Resting Value |
| I | 2 | Moderate Claudication | Between Categories 1 and 3 |
| I | 3 | Severe Claudication | Cannot Complete Treadmill Exercise
AP < 50 mmHg After Exercise |
| II | 4 | Ischemic Rest Pain | Resting AP < 30-50 mmHg
TP < 30 mmHg Ankle/Metatarsal PVR Flat or Barely Pulsatile |
| III | 5 | Minor Tissue Loss | Resting AP < 50-70 mmHg
TP < 40 mmHg in Nondiabetics TP < 50 mmHg in Diabetics Ankle/Metatarsal PVR Flat or Barely Pulsatile tcPO2 < 30 mmHg |
| III | 6 | Major Tissue Loss | Same as Category 5 |
- *AP – Ankle Pressure, TP – Toe Pressure, PVR – Pulse Volume Recording, tcPO2 – Transcutaneous Oxygen
Other Systems
- Bollinger Classification – Based on Angiographic Description
- Graziani Classification – Anatomic Classification in Diabetic Foot Ulcers
- Trans-Atlantic Inter-Society Consensus (TASC II) – Describes Anatomic Classification of Disease
Peripheral Arterial Disease (PAD) – Treatment
Management Approach
- Intermittent Claudication
- Initial Tx: Medical Management
- If Fails & Lifestyle-Limiting: Endovascular Revascularization
- May Consider Surgical Revascularization in Select Cases
- Chronic Limb-Threatening Ischemia
- Preferred Tx: Revascularization (Endovascular or Surgical)
- Amputation Indications:
- Overwhelming Infection
- Vascular Disease Unable to be Reconstructed
- Consider Medical Management Alone if:
- Superficial Ulceration with Vascular Disease Unable to be Reconstructed to Avoid Amputation
- Avoid Major Amputation in High-Risk Patients Near End-of-Life
- Acute Limb Ischemia
Medical Management
- Smoking Cessation #1
- Exercise Therapy
- Most Effective Exercise: Treadmill or Track Walking
- Resistance Training Beneficial but Should Not Substitute
- Exercise Beyond Initial Onset of Pain, Until Pain is Moderate-Severe – Increases Collaterals
- Most Effective Exercise: Treadmill or Track Walking
- Antiplatelet Therapy (Aspirin/Clopidogrel)
- Statin
- Medications for Intermittent Claudication Symptomatic Relief:
- Cilostazol (Pletal)
- PDE3 Inhibitor/Vasodilator Provides Symptomatic Relief
- Contraindicated if History of Congestive Heart Failure
- Pentoxifylline
- Methylxanthine Derivative Improves Oxygen Delivery by Enhancing RBC Deformability
- Can Interfere with Blood Clotting/Coumadin
- Cilostazol (Pletal)
Aortoiliac Disease Revascularization
- Endovascular Angioplasty & Stenting
- Used with Increasing Frequency
- Previously Limited to Short-Segment TASC A/B Lesions but Now Being Used for Even Longer-Segment Lesions
- Relative Contraindications:
- Extensive Aortic/Renal Involvement
- Heavy Calcification – Risk Rupture
- Poor Renal Function (Unless Already on Dialysis – Will Clear Contrast)
- Aortofemoral/Aortobifemoral Bypass
- Gold Standard Surgical Procedure
- Axillofemoral/Axillobifemoral Bypass
- Possible Indications:
- “Hostile” Abdomen
- Stoma Presence
- Infected Grafts
- Prior Radiation
- Possible Indications:
- Iliofemoral Bypass
- Femorofemoral (Fem-Fem) Bypass
- Aortoiliac Endarterectomy
Infrainguinal (Femoropopliteal/Tibioperoneal) Disease Revascularization
- Endovascular Angioplasty & Stenting
- Preferred Approach
- Relative Contraindications:
- Long Segment Stenosis/Occlusion
- Multifocal Stenosis
- Eccentric Calcified Stenosis
- Surgical Bypass
- Common Femoral Endarterectomy
- Poor Access at Other Sites
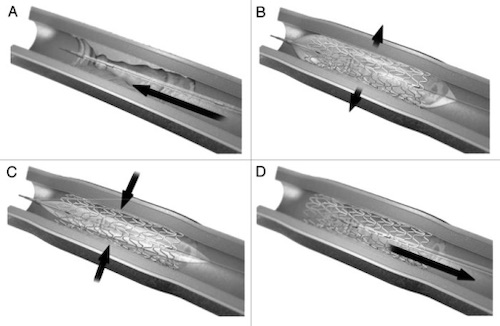
Endovascular Stent Placement; (A) Stent Mounted on Catheter, (B) Balloon Inflated and Stent Expanded, (C) Balloon Deflated, (D) Catheter Removed 3

Axillobifemoral Bypass 4

Femorofemoral Bypass 5

Femoral Endarterectomy 6
Upper Extremity Stenosis
Basics
- Much Less Common than Lower Extremity Disease
- Upper Extremity Disease is More Likely Caused by Autoimmune or Connective Tissue Disease
- Atherosclerosis is Not as Significant as Lower Extremity Disease
- Most Common Site: Subclavian
Presentation
- Proximal Disease is Usually Asymptomatic from Collaterals
- Intermittent Pain with Use
- Ischemic Resting Pain, Particularly in the Digits
- Ulceration & Gangrene
- Critical Limb Ischemia
- Muscle Atrophy
Associated Syndromes
- Subclavian Steal Syndrome
- Reverse Flow Through Vertebral Artery from Proximal Subclavian Stenosis
- Causes Limb & Vertebrobasilar Symptoms
- Coronary-Subclavian Steal Syndrome
- After CABG with LIMA
- Retrograde Flow Through LIMA to Subclavian
Upper Extremity Disease Revascularization
- Endovascular Angioplasty & Stenting
- Utilized Less Frequently than in Lower Extremity Disease
- Surgical Bypass
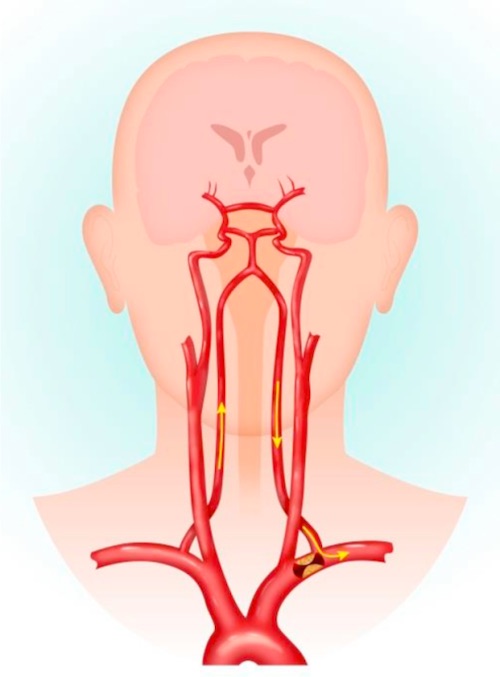
Subclavian Steal Syndrome 7
References
- Khwaja HA, Omotoso PO. Bifurcated Dacron patch for simultaneous superficial femoroplasty and profundoplasty: a case report. J Med Case Rep. 2009 Nov 24;3:9294.(License: CC BY-2.0)
- Wu G, Yang J, Zhang T, Morelli JN, Giri S, Li X, Tang W. The diagnostic value of non-contrast enhanced quiescent interval single shot (QISS) magnetic resonance angiography at 3T for lower extremity peripheral arterial disease, in comparison to CT angiography. J Cardiovasc Magn Reson. 2016 Oct 20;18(1):71. (License: CC BY-4.0)
- Bhat S, Kumar A. Biomaterials and bioengineering tomorrow’s healthcare. Biomatter. 2013 Jul-Sep;3(3):e24717. (License: CC BY-NC-3.0)
- Zhang JL, Yang SM, Yao Q, Chen JH, Wang T, Wang H, Fan J, Ling R, Yi J, Yuan SF, Wang L. Palliative surgery for primary sarcoma in the abdominal aorta: A case report and review of the literature. Oncol Lett. 2013 Dec;6(6):1738-1740. (License: CC BY-3.0)
- Kang SH, Bae JM, Yun WS. Endovascular aortic aneurysm repair using a bifurcated stent graft in a patient with femoro-femoral bypass. Ann Surg Treat Res. 2015 Aug;89(2):107-10. (License: CC BY-NC-3.0)
- Rocha-Singh KJ, Zeller T, Jaff MR. Peripheral arterial calcification: prevalence, mechanism, detection, and clinical implications. Catheter Cardiovasc Interv. 2014 May 1;83(6):E212-20.(License: CC BY-NC-3.0)
- Konda S, Dayawansa S, Singel S, Huang JH. Pseudo subclavian steal syndrome: Case report. Int J Surg Case Rep. 2015;16:177-80.(License: CC BY-NC-ND-4.0)