Vascular: Peripheral Revascularization
Vascular Bypass
Conduits
- Autologous Vein Grafts (AVG) – Preferred if Available
- Great Saphenous Vein (GSV)
- GSV is the Best Choice
- Small Saphenous Vein (SSV)
- Femoral Vein
- Basilic Vein
- Cephalic Vein
- *AVG Required Diameter: 3 mm Minimum, 4 mm Ideally
- Great Saphenous Vein (GSV)
- Prosthetic Grafts
- Polytetrafluoroethylene (PTFE) – Gortex
- Dacron – Polyester Fabric
Preferred Bypass Choice
- Aortoiliac Disease: Dacron – Generally Preferred with Proven Durability
- *Some Prefer PTFE
- Infrainguinal Disease: Autologous Vein Graft – GSV Best
- If AVG Unavailable: PTFE (Poor Patency if Below the Knee)
Bypass Route
- Axillofemoral Bypass
- Axillary-Femoral & Femoral-Femoral Bypasses
- Extra-Anatomic Bypass
- Can Avoid Hostile Abdomen (Such as Multiple Previous Surgeries)
- 5-Year Patency: 75%
- If Used for Graft Infection:
- Right-Side is Preferred – Allows Preservation of Left Flank for Retroperitoneal Exposure
- Bypass is Performed Prior to Infected Graft Resection
- Aortobifemoral Bypass
- Split Bypass from the Aorta to Both Femoral Arteries
- Approach:
- Transperitoneal
- Traditional
- Retroperitoneal
- Allows Avoidance of Intraabdominal Adhesions
- Provides Greater Access to the Visceral Abdominal Aorta Such as the Left Renal Artery
- Increased Pain, Flank Wall Laxity and Risk for Hernia
- Transperitoneal
- Risk Vasculogenic Impotence & Pelvic Ischemia
- Proximal/Aortic Anastomosis: (Debated)
- End-to-End:
- Coexisting Aneurysmal Disease
- Complete Aortic Occlusion
- End-to-Side:
- Avoid Sacrifice of a Large IMA
- Bilateral External Iliac Occlusion – Avoid Pelvis Devascularization (No Retrograde Flow)
- End-to-End:
- Must Ensure Backflow in At Least One Internal Iliac & Hypogastric
- If No Backflow: Bypass to Internal Iliac Also
- 5-Year Patency: 90-95%
- Bilateral Bypasses Have Higher Patency Rates Compared to Unilateral Counterparts Due to Higher Outflow
- Femoral-Femoral Crossover
- Bypass from One Femoral Artery to the Contralateral Femoral Artery
- Risk Vascular Steal in the Donor Leg
- Femoropopliteal Bypass
- Bypass from the Femoral Artery to the Popliteal Artery
- Distal Site: Popliteal Below Knee (Between Gastrocnemius and Popliteus)
- Femoral-Distal Grafts
- Options: Peroneal, Anterior Tibial or Posterior Tibial
- Preferred Conduit: Ipsilateral Greater Saphenous Vein
- Only for Limb or Tissue Salvage (Non-Healing Ulcer)
- Higher Risk of Limb Loss
- From Lack of Collaterals
Complications
- Reperfusion Injury
- Definition: Tissue Damage After Reperfusion
- Cause: Inflammation and Oxidative Damage in Previously Ischemic Site
- Oxygen Radical Cause Increased Extravasation into Tissues & Swelling
- Primary Mediator: PMN’s (Neutrophils)
- Presentation:
- Compartment Syndrome
- Lactic Acidosis
- Hyperkalemia
- Myoglobinuria
- Most Common Causes of Bypass Failure:
- Early (< 1 Month): Technical Error
- Intermediate (1 Month-2 Years): Intimal Hyperplasia
- Late (> 2 Years): Atherosclerosis
- Bypass Graft Infection
- Most Common Organisms
- Early: S. aureus
- Late: S. epidermidis (Biofilm)
- General Treatment: Graft Excision & Non-Anatomic Graft Placement
- Most Common Organisms
- Most Common Cause of Postoperative Edema: Lymphocele

Axillobifemoral Bypass 1

Femorofemoral Bypass 2
Vascular Stenting
Stent Types
- Balloon-Expandable
- High Radial Force
- Low Flexibility
- Very Precise in Deployment
- Self-Expanding
- Low Radial Force – Force Required to Create a 50% Reduction in Stent Diameter
- High Flexibility
Other Considerations
- Bare-Metal Stent (BMS)
- Simple Metal/Metal-Alloy Framework
- Drug-Eluting Stent (DES)
- Contain a Durable Polymer & Anti-Stenotic Drug (Everolimus, Zotarolimus, Sirolimus, etc.)
- Inhibit Neointimal Response (Early Failure)
- Possibly Higher Risk of Late Failure
- Covered Stent (Stent Graft)
- Stent Covered by ePTFE, Polyurethane or Silicone
- Permit Complete Exclusion of Vessel Defects
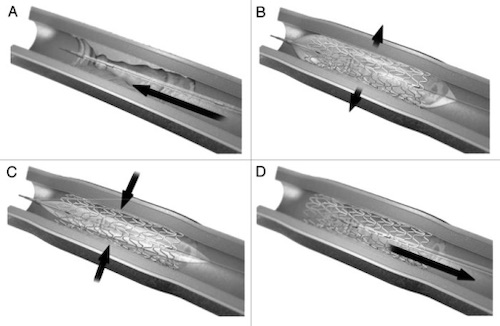
Endovascular Stent Placement; (A) Stent Mounted on Catheter, (B) Balloon Inflated and Stent Expanded, (C) Balloon Deflated, (D) Catheter Removed 3
Femoral Endarterectomy
Basics
- Mostly Replaced by Endovascular Techniques
- Typically Only Used for Short-Segment Focal Lesions of the SFA when Not Amenable to Endovascular Treatment or Lacking Adequate Vein Conduit
Procedure Considerations
- Divide Lateral Femoral Circumflex Vein
- Travels Between SFA/DFA
- Risk for Injury if Left
- Close with a Patch Angioplasty

Femoral Endarterectomy 4
References
- Zhang JL, Yang SM, Yao Q, Chen JH, Wang T, Wang H, Fan J, Ling R, Yi J, Yuan SF, Wang L. Palliative surgery for primary sarcoma in the abdominal aorta: A case report and review of the literature. Oncol Lett. 2013 Dec;6(6):1738-1740. (License: CC BY-3.0)
- Kang SH, Bae JM, Yun WS. Endovascular aortic aneurysm repair using a bifurcated stent graft in a patient with femoro-femoral bypass. Ann Surg Treat Res. 2015 Aug;89(2):107-10. (License: CC BY-NC-3.0)
- Bhat S, Kumar A. Biomaterials and bioengineering tomorrow’s healthcare. Biomatter. 2013 Jul-Sep;3(3):e24717. (License: CC BY-NC-3.0)
- Rocha-Singh KJ, Zeller T, Jaff MR. Peripheral arterial calcification: prevalence, mechanism, detection, and clinical implications. Catheter Cardiovasc Interv. 2014 May 1;83(6):E212-20.(License: CC BY-NC-3.0)