Skin & Soft Tissue: Plastics & Tissue Transfer
Definitions
Tissue Transfer Definitions
- Flap: Tissue Transfer with an Intact Blood Supply
- Graft: Tissue Transfer without an Intact Blood Supply
Complex Defect Reconstructive Ladder (Simple to Complex)
- Secondary Intention
- Primary Closure
- Skin Graft
- Local Flap
- Regional Flap
- Free Flap
Flaps
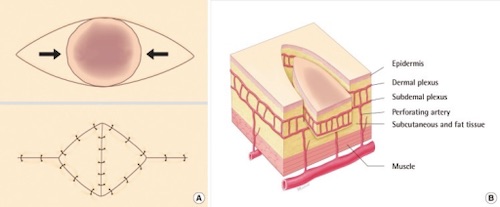
Blood Supply
- Pedicled Flap: Pedicle of Donor Site with Vascular Supply Remains Intact
- Free Flap: Tissue Completely Detached from Donor Site
- Blood Supply Reconstituted at Recipient Site by Microsurgery
- Microvascular Free Flap Survival: 95%
Proximity
- Local Flap: Uses Tissue That Abuts the Defect
- Types
- Advancement Flap: Tissue Stretched in a Straight Line
- Ex: V-Y Flap
- Rotational Flap: Tissue Stretched in an Arc
- Transposition Flap: Tissue Rotated, Creating a New Defect
- Ex: Rhomboid Flap or Z-Plasty
- Advancement Flap: Tissue Stretched in a Straight Line
- Types
- Regional Flap: Uses Tissue Near the Defect that Does Not Actually Abut the Defect
- Still Connected to Donor Site by Pedicle
- Interpolation Flap: A 2-Stage Regional Flap
- First the Flap is Transferred Keeping a Pedicle Connected to the Donor Site Over/Under a Skin Bridge
- Later the Pedicle is Removed After Neovascularization
- Distant Flap: Uses Tissue Far from the Defect
- Can Be Pedicled or Free Flap
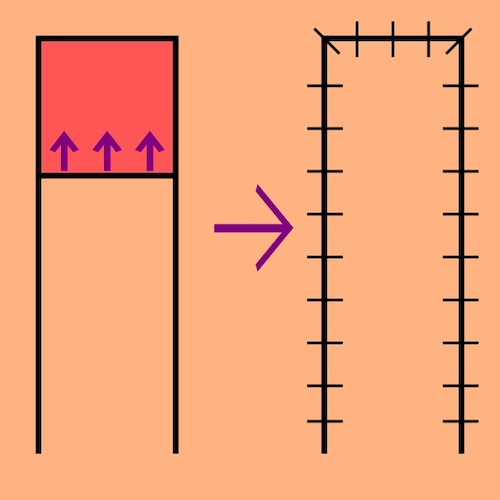
Advancement Flap 1
V-Y Advancement Flap 2
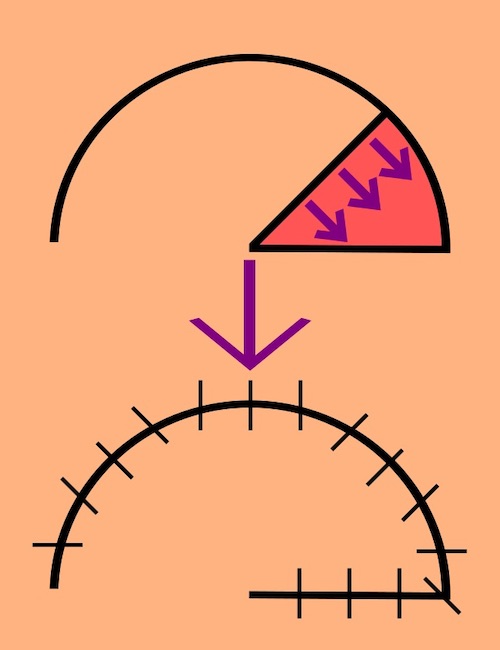
Rotational Flap 1
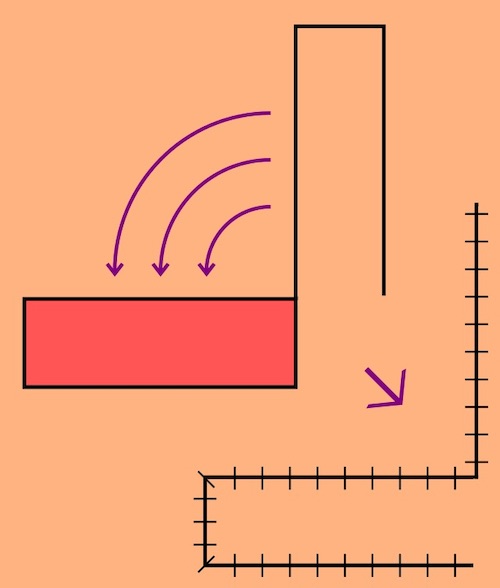
Transposition Flap 1
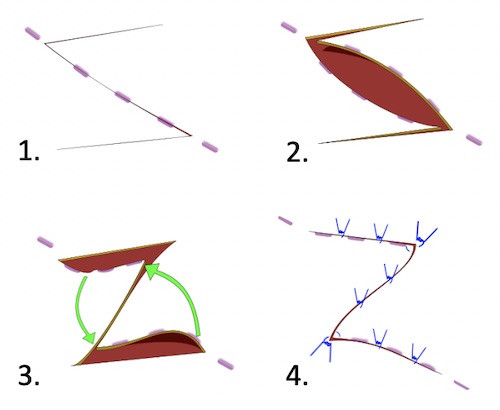
Z-Plasty 3
Common Flaps
- Breast Reconstructions:
- Transverse Rectus Abdominis Myocutaneous (TRAM) Flap
- Deep Inferior Epigastric Perforator (DIEP)/Fasciocutaneous Flap
- Superficial Inferior Epigastric Artery (SIEA) Flap
- Latissimus Dorsi Myocutaneous Flap (LDMF)
- Thoracodorsal Artery Perforator Flap (TDAP)
- *See Breast: Breast Reconstruction
- Other Common Flaps:
- Forehead Flap
- Omental Flap
- Anterolateral Thigh Flap
- Radial Forearm Flap
- Medial Gastrocnemius Flap
Grafts
Types of Grafts
- Autograft
- Definition: Graft from the Same Patient Themselves
- Best Outcomes
- Allograft/Homograft
- Definition: Graft from Another Human or Cadaver
- Decellularized & Rendered Nonimmunogenic by Washing Process
- Will Vascularize
- Temporize (4 Weeks) – Will Eventually Reject & Must be Replaced
- Definition: Graft from Another Human or Cadaver
- Xenograft
- Definition: Acellular Collagen Extracts from Nonhuman Sources (Porcine or Bovine)
- No Vascularization
- Temporize (2 Weeks)
- Dermal Substitute
- Uses Synthetic Materials (Vicryl, PTFE, Prolene, etc.)
- Worst Outcomes
Autograft Thickness
- Split-Thickness Skin Graft (STSG)
- Layers: Epidermis & Superficial Dermis
- Most Likely to Survive (Thin with Better Imbibition)
- Donor Site Heals by Edges & Hair Follicles After 1-2 Weeks
- Harvest with a Dermatome
- If Too Deep: Stop, Suture Repair & Start at Another Site
- Meshing:
- Increases Tissue Coverage & Decreases Amount Harvested
- Allows Drainage of Fluid/Blood (Lower Seroma/Hematoma Risk)
- Heals by Secondary Intention Between Gaps
- Increased Scarring & Longer Healing Time
- Full-Thickness Skin Graft (FTSG)
- Layers: Epidermis & All of Dermis (No Subcutaneous)
- Remove Fat to Avoid Fat Necrosis & Facilitate Revascularization
- Less Contraction
- Generally Only Used for Small Areas for Cosmetics/Function (Such as Face or Hand)
- Potential Donor Sites: Post-Auricular, Supraclavicular, Lateral Neck, Inner Arms, Forearms & Inguinal Crease
- Choose Site with Best Cosmetic Match
- Harvest with a Knife & Close Donor Site Primarily (Will Not Heal)
- Layers: Epidermis & All of Dermis (No Subcutaneous)
Graft Survival
- Initial: Imbibition
- Osmotic Diffusion
- Day 3-4: Inosculation
- Direct Connection to Wound Bed Vessels
- Day 5: Neovascularization
- Formation of New Blood Vessels with Angiogenesis
Contraction
- Primary Contraction
- Occurs Immediately at the Time of Harvest
- Caused by Elastic Recoil of Dermis
- Directly Proportional to the Amount of Dermis
- Higher in FTSG
- Secondary Contraction
- Delayed Contraction
- Caused by Healing Skin & Host Bed Contraction
- Inversely Proportional to the Amount of Dermis
- Higher in STSG
Causes of Graft Failure
- Hematoma/Seroma of Wound Bed – Most Common Cause
- Prevents Nutrient Delivery & Neovascularization
- Infection
- Poor Wound Bed/Vascularity
- Sheer Forces
Donor Site Management
- Must Achieve Adequate Hemostasis – High Risk for Significant Blood Loss
- Moist Environments are Generally Preferred
- Options: Xeroform, Petroleum-Impregnated Gauze or Alginate
- Moist Environments Improve Wound Healing & Decrease Pain
- Dry Gauze Causes Pain When Changing
- Leaving Open to Air Increases Risk of Infection
- Scarring is Expected
- Donor Site is Generally More Painful than the Recipient Site

Skin Graft Dermatome 4

Dermacarrier & Mesher 5

Meshed STSG 6
References
- Taylornate. Wikimedia Commons. (License: CC BY-SA-3.0)
- Kwon KH, Lee DG, Koo SH, Jo MS, Shin H, Seul JH. Usefulness of v-y advancement flap for defects after skin tumor excision. Arch Plast Surg. 2012 Nov;39(6):619-25. (License: CC BY-NC-3.0)
- Mason E. Wikimedia Commons. (License: CC BY-SA-4.0)
- Miller JD, Rankin TM, Hua NT, Ontiveros T, Giovinco NA, Mills JL, Armstrong DG. Reduction of pain via platelet-rich plasma in split-thickness skin graft donor sites: a series of matched pairs. Diabet Foot Ankle. 2015 Jan 22;6:24972. (License: CC BY-NC-ND-3.0)
- Wokes JE, Ali-Khan A. Microfenestrated split thickness skin grafts: an underused technique? Ann R Coll Surg Engl. 2012 Sep;94(6):447. (License: CC BY-3.0)
- Sakamoto, Y., & Kishi, K. (2013). The Fixation and Dressing for Meshed and Sheet Skin Graft. In (Ed.), Skin Grafts. IntechOpen. (License: CC BY-3.0)