Large Intestine: Appendicitis
Appendicitis
Appendix Physiology
- Luminal Capacity of 1 cc
- Secretes IgA
- Function: Reservoir for Good Bacteria After Infection Cleans Out
- *Previously Thought to Be a Vestigial Structure
- “Vermiform Appendix” Simply References the “Worm-Like” Appearance
- Positioning:
- Retrocecal (64%) – Behind the Cecum (Most Common)
- Subcecal (32%) – Inferior to & Extending from the Cecum
- Pelvic (2%) – Within Pelvis
- Preileal (1%) – Anterior to Ileum
- Postileal (0.5%) – Posterior to Ileum
- Blood Supply: Appendicular Artery within Mesoappendix (Off the Ileocolic Artery
Appendicitis Pathology
- Lifetime Risk of Developing: > 15%
- Cause: Luminal Obstruction & Stasis
- Most Common Cause:
- Peds: Lymphoid Hyperplasia
- Adults: Appendicolith (Fecalith at the Appendiceal Orifice)
- Leads to:
- Swelling and Mucous Secretion
- Impaired Blood Flow & Venous Congestion
- Bacterial Infection
- Can Progress to Ischemia & Necrosis
- Most Common Cause:
- Most Common Parasite: Ascariasis lumbricoides
Complicated Appendicitis
- Definition: Acute Inflammation of the Peritoneum Secondary to Infection of the Appendix
- Types:
- Periappendicular Phlegmon
- Periappendicular Abscess
- Perforated Appendicitis
Perforation
- 13-20% Present with Perforation
- Can be a Contained Walled-Off Abscess or Free Perforation
- More Common if Presenting After 24 Hours of Symptom Onset
- Most Common Perforation Site: Midpoint on Antimesenteric Border
- Risk Factors for Perforation:
- Age < 4 Years
- Symptom Duration > 48 Hours
- Immunodeficiency
- Hispanic, Black or Asian Race
- Self-Insured or Public Insurance
Presentation
- Initial Periumbilical Pain that Migrates to the RLQ (75% Demonstrate Migration)
- Initial Umbilical Pain Caused by Visceral Peritoneal Fibers from Appendix Stretching
- Migrating RLQ Pain Caused by Parietal Somatic Fibers from Peritoneal Inflammation
- Pain Worse with Walking, Jumping or Coughing
- Anorexia (92%)
- Nausea (78%)
- Nausea & Anorexia Occur After Pain Once Secondary Visceral Afferent Fibers Stimulate the Medullary Vomiting Center (Occurs Before Pain in Gastroenteritis)
- Vomiting (67%)
- Fever
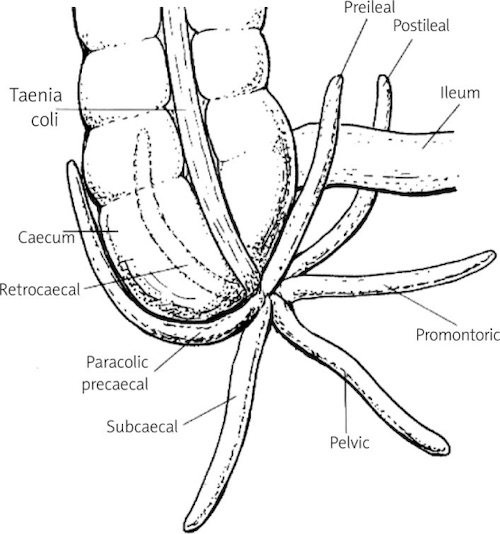
Appendix Positions 1
Diagnosis
Physical Exam Signs Mn
- McBurney Sign
- RLQ Tenderness at McBurney’s Point (1/3 Distance from ASIS to Umbilicus)
- Most Reliable Finding
- Rovsing Sign
- RLQ Pain on LLQ Palpation
- Iliopsoas/Psoas Sign
- Pain on Extension of Right Thigh
- Indicates: Retrocecal Appendix
- Obturator Sign
- Pain on Internal Rotation of Right Thigh
- Indicates: Pelvic Appendix
- Likely to Cause Dysuria & Diarrhea
Scoring Systems
- Alvarado/MANTRELS Scoring System
- Used in Adults, Poor Accuracy in Peds
- Points:
- Migration to RLQ (1)
- Anorexia (1)
- Nausea/Vomiting (1)
- RLQ Tenderness (2)
- Rebound (1)
- Elevated Temperature (1)
- Leukocytosis (2)
- Shift of Neutrophils (1)
- Low Scores (0-3) Are Better to “Rule-Out” Appendicitis than High Scores (7-10) Are to Rule In
- Low Scores (0-3): Evaluate Other Etiologies
- Intermediate-High Scores (4-10): Further Appendicitis Evaluation & Imaging
- Pediatric Appendicitis Score (PAS)
- Used for Peds
- Points:
- RLQ Tenderness (2)
- Pain with Cough, Percussion or Hopping (2)
- Anorexia (1)
- Nausea/Vomiting (1)
- Migration of Pain (1)
- Fever (1)
- Leukocytosis > 10,000 (1)
- Neutrophils Plus Band Forms > 7,500 (1)
- Risk/Scores
- Low Scores (0-3): Evaluate Other Etiologies
- 0-2% Risk
- Intermediate Scores (4-6): Imaging
- 8-48% Risk
- High Scores (7-10): Imaging vs Surgery
- 78-96% Risk
- Low Scores (0-3): Evaluate Other Etiologies
- Refined Low-Risk Appendicitis Score
- Used to Rule Out Appendicitis in Peds
- Factors:
- Absence of Maximal Tenderness in RLQ OR RLQ Tenderness without Pain on Walking, Jumping or Coughing
- ANC < 6,750
- 98% Sensitive & 95% Negative Predictive Value in Identifying Peds without Appendicitis
Diagnosis
- Adults: CT
- Peds or Pregnant Women: US
- If Equivocal Consider MRI (Often Preferred) vs CT
- Radiographic Findings:
- Appendix Distended ≥ 6-7 mm
- Wall Thickening ≥ 3 mm & Noncompressible
- Appendicolith (10%) – Increases Risk for Complicated Appendicitis
- Periappendiceal Fluid & Fat Stranding

Appendicitis with Fecalith

Perforated Appendicitis
Treatment
Definitive Management
- Uncomplicated: Appendectomy
- Complicated (Phlegmon/Abscess): ABX & Interval Appendectomy at 6-8 Weeks
- Percutaneous Drainage if Abscess > 3-4 cm
- ABX Course:
- After Percutaneous Drainage: 4 Days
- If Unable to Perform Percutaneous Drainage: 7 Days
- Immediate Appendectomy:
- Increased Risk of Complications (SBO, Prolonged Ileus, Surgical Site Infection & Reoperation)
- May Have Earlier Return to Activity (Debated)
- Risk of Recurrence: 5-38% (Same as General Population)
- *Some Recommend No Appendectomy Due to Low Recurrence Rate, Although the Most Compelling Reason for Interval Appendectomy is the Risk of Neoplasm After Perforation
- Free Perforation: Appendectomy
Intraoperative Findings
- Normal Appendix: Always Resect (As Long as Cecum Not Inflamed)
- Prevent Risk of Diagnostic Confusion in the Future
- Friable Base: Partial Cecectomy; Preserve Ileocecal Valve
- Suspect Chron’s Disease & Cecum Inflamed: No Intervention
Nonoperative Management
- Some Promote ABX Treatment Alone for Uncomplicated Acute Appendicitis
- *In General, Surgical Management is Preferred but May Consider if Unfit for Surgery or Refuses Surgery
- Benefits:
- Most Respond Clinically
- Faster Return to Work (Not for Complicated/Perforated Cases)
- No Increased Perforation Rate
- 89-91% Are Able to Avoid Surgery at Initial Admission
- Negatives:
- High Recurrence
- 29% Require Appendectomy by 90 Days
- 25% Without Appendicolith
- 41% With Appendicolith
- 14-37% Require Appendectomy within the First Year
- Additional 16% Require Appendectomy Between 1-5 Years
- 29% Require Appendectomy by 90 Days
- Tx Efficacy at 1-Year:
- Nonoperative Management: 63.8%
- Surgical Management: 93%
- Contraindicated if Fecalith Present – High Rate of Complicated Appendicitis that May be Underestimated on Imaging
- High Recurrence
- Immunocompromised & Significant Comorbidity Patients Have Mostly Been Excluded from Prior Studies with Uncertain Efficacy
Incidental Appendectomy
- Appendectomy During Another Separate Procedure without Evidence of Appendicitis
- Indications:
- Peds About to Undergo Chemo
- Paraplegic
- Chron’s
- About to Travel to Remote Places

Laparoscopic Appendectomy 2
Special Populations
Pediatrics
- Higher Rate of Perforation & Morbidity (Due to Delayed Diagnosis)
- Underdeveloped Omentum – Harder to Wall Off Abscess
Pregnancy
- The Most Common Non-Obstetric Indication for Surgery During Pregnancy
- Only 50-60% Have a Classical Clinical Presentation
- Location of Pain:
- RLQ in First Two Trimesters
- RUQ by Third Trimester
- Risk:
- Nonperforated – 1.5-2.0% Fetal Loss, 6% Preterm Labor
- Complicated – 8-36% Fetal Loss, 11% Preterm Labor
- Highest Risk for Fetal Mortality: Rupture
- Considerations by Trimester
- First – Most Common Cause of Acute Abdominal Pain
- Second – Most Frequent Trimester
- Third – Most Likely to Perforate
- Tx: Appendectomy
- Laparoscopic Approach Still Preferred
- *Previously Concerned for Increased Risk of Fetal Loss/Preterm Labor Now Relieved
- Trocar Placement: *See Large Intestine: Appendectomy
- If Preforming Open Make Incision at the Site of Pain (More Cephalad)
- Laparoscopic Approach Still Preferred
HIV/AIDS
- More Frequent
- Present Later – Increased Risk of Rupture
Similar Pathology
Mesenteric Lymphadenitis (Pseudoappendicitis)
- Mesenteric Lymph Node Inflammation
- Presents Similar to Appendicitis
- Most Common in Peds
- Causes:
- Viral Upper Respiratory Infection (URI) – Most Common
- Gastroenteritis
- Inflammatory Bowel Disease
- Lymphoma
- Tx: None (No Bx Needed)
- Resolves Over 1-10 Weeks
Periappendicitis
- Appendiceal Serosal Inflammation without Mucosal Inflammation
- Caused by Non-Appendiceal Inflammation
- Presents Similar to Appendicitis
- Causes:
- Salpingitis – Most Common
- Distant Perforation Elsewhere
- Pelvic Inflammatory Disease (PID)
- Peritoneal Tuberculosis
- Inflammatory Bowel Disease (IBD)
- Valentino’s Syndrome – Peri-Appendicitis Caused by a Perforated Gastric/Duodenal Ulcer
Appendiceal Mucocele (Non-Neoplastic Mucinous Lesion/Retention Cyst)
Appendix Cancer
Mnemonics
Signs of Appendicitis
- McBurney Sign – “Burns” Right Over the Appendix
- Rovsing Sign – Think “Roving” Pain Elicited from a Distant Site
- Psoas Sign (Pso-Po) – Posterior (Retrocecal)
- Obturator Sign (Ob-Ob) – Obstetrics (Pelvic Location & Internal Rotation to Pelvis)
References
- Bakar SM, Shamim M, Alam GM, Sarwar M. Negative correlation between age of subjects and length of the appendix in Bangladeshi males. Arch Med Sci. 2013 Feb 21;9(1):55-67.(License: CC BY-NC-ND-3.0)
- Strzałka M, Matyja M, Rembiasz K. Comparison of the results of laparoscopic appendectomies with application of different techniques for closure of the appendicular stump. World J Emerg Surg. 2016 Jan 6;11:4. (License: CC BY-4.0)