Large Intestine: Colon Cancer
Colon Cancer
General
- Third Most Common Cancer Diagnosis
- Third Most Common Cancer Death
- Lifetime Risk:
- Males: 1/22 (4.49%)
- Females: 1/24 (4.15%)
- Most Common Site: Sigmoid Colon
Risk Factors
- Obesity & Physical Inactivity
- Diet High in Red Meat, Processed Meat & Fat
- Tobacco & Alcohol
- Clostridium septicum
- Inflammatory Bowel Disease
- Genes: APC, DCC, p53, K-Ras
- APC is Present in 80% of Sporadic Colon Cancers (No Increased Risk of FAP)
- *Aspirin May Provide Protection from Development of Colorectal Cancer by Inflammatory Pathway (COX/LOX) Inhibition
Associated Genetic Syndromes
- *See Oncology: Colorectal Cancer & Polyposis Syndromes
- Familial Adenomatous Polyposis (FAP)
- Includes:
- Gardner’s Syndrome
- Turcot’s Syndrome
- Includes:
- Lynch Syndrome (Hereditary Nonpolyposis Colon Cancer/HNPCC)
- Familial Juvenile Polyposis
- Mut Y Homolog-Associated Polyposis (MAP)
- Peutz-Jeghers Syndrome
- PTEN Hamartoma Tumor Syndrome
- Includes:
- Cowden Syndrome
- Bannayan-Riley-Ruvalcaba Syndrome
- Cronkhite-Canada Syndrome
- Includes:
- Serrated Polyposis Syndrome
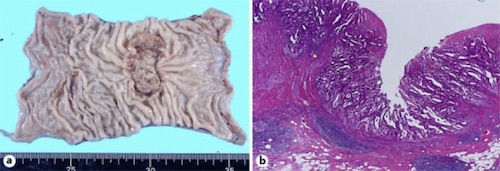
Sigmoid Adenocarcinoma 1

FAP 2
Appendix-Specific Considerations
- Adenocarcinoma
- Most Common Presentation: Acute Appendicitis
- Mucinous Adenocarcinoma – Most Common Source of Pseudomyxoma Peritonei
- Carcinoid Tumor
- Most Common Tumor of the Appendix
- *See Small Intestine: Carcinoid Tumor
Prognosis
- Most Important Staging Factor: Nodes
- Lymphocytic Reaction/Penetration – Improves Prognosis
- Improved Prognosis:
- High Microsatellite Instability (MSI-H)
- Deficient DNA Mismatch Repair (dMMR)
- Lymphocytic Reaction/Penetration
- Poor Prognostic Factors:
- Microsatellite Stable (MSS)
- Proficient DNA Mismatch Repair (pMMR)
- Lymphovascular Invasion
- Mutations – KRAS, NRAS or BRAF
- 5-Year Survival (By AJCC 7):
- Stage I: 74.1%
- Stage II:
- A: 64.5%
- B: 51.6%
- C: 32.3%
- Stage III:
- A: 74.0% (Higher Than Stage II)
- B: 45.0%
- C: 33.4%
- Stage IV: 6%
- Resectable Liver Mets: 35% (Higher)
- Resectable Lung Mets: 25%
Recurrence/Mets
- Best Test for Intrahepatic Lesions: Intraoperative US (3-5 mm Resolution)
- Rates of Distant Colorectal Lesions:
- Synchronous Benign Polyps: 12-62%
- Synchronous Cancers: 2-8%
- Metachronous Cancer: 25-30%
- Recurrence:
- 20% Have Recurrence (Most Within First Year)
- 5% Get A New Primary
- Rectal CA Higher Risk of Recurrence Than Colon CA
- Mets:
- Most Common Site: Liver (Portal Vein)
- Second Most Common Site: Lung (Iliac Vein)
- Spinal Mets are from the Rectum (Batson’s Plexus) – Not Colon
Presentation
- Mostly Asymptomatic When in Early Stages – Diagnosed Through Routine Screening
- Symptoms:
- GI Bleeding – Most Common Initial Symptom
- Iron Deficiency Anemia
- Constipation or Obstruction – More Common on the Left-Side
- Abdominal Pain
Preoperative Evaluation
- Total Colonoscopy
- To Evaluate for Synchronous Lesions
- Endoscopic Tattoo to Ease Surgical Resection
- CT Chest/Abdomen/Pelvis
- Evaluate Mets
- Labs (CBC/CMP)
- Carcinoembryonic Antigen (CEA)
- Used to Monitor for Recurrent Mets
- CEA Itself is Not Diagnostic of Colon Cancer
- Poor Sensitivity for Local Recurrence
- Should Check for a Baseline Level Preoperatively & Follow Postoperatively
- CEA is Produced by Normal Tissues in Development but Stops Before Birth
- Used to Monitor for Recurrent Mets
TNM Staging
- TNM
| T | N | M | |
| 1 | Submucosa | 1a – 1
1b – 2-3 1c – Discrete Tumor Nodules in Lymph Drainage Area without Identifiable Lymph Node Tissue |
1a – One Distant Organ
1b – ≥ 2 Distant Organs 1c – Peritoneal Mets |
| 2 | Into Muscularis Propria | 2a – 4-6 LN
2b – ≥ 7 LN |
|
| 3 | Into Serosa | ||
| 4 | 4a – Through Serosa
4b – Into Adjacent Tissue/Organs |
- Staging
| T | N | M | ||
| I | T1-2 | N0 | M0 | |
| II | A | T3 | N0 | M0 |
| B | T4a | N0 | M0 | |
| C | T4b | N0 | M0 | |
| III | A | T1 | N1-2a | M0 |
| T2 | N1 | M0 | ||
| B | T1 | N2b | M0 | |
| T2 | N2 | M0 | ||
| T3 | N1-N2a | M0 | ||
| T4a | N1 | M0 | ||
| C | T3 | N2b | M0 | |
| T4a | N2 | M0 | ||
| T4b | N1-2 | M0 | ||
| IV | A | Any T | Any N | M1a |
| B | Any T | Any N | M1b | |
| C | Any T | Any N | M1c | |
Colon Cancer – Treatment
Initial Management
- Surgery is the Mainstay of Treatment
- Criteria that Endoscopic Excision is Sufficient: Mn
- T1 (< T2)
- > 2 mm Margin
- Well Differentiated
- No Vascular or Lymphatic Invasion
- Complicated Presentation:
- Presenting with Obstruction: Consider Oncologic Resection vs Temporization with Delayed Elective Surgery
- Temporizing Options:
- Loop Transverse Colostomy
- Colonic Stent
- Temporizing Options:
- Presenting with Perforation: Normal Oncologic Resection with Complete Mesocolic Excision
- Strongly Consider Ostomy
- Presenting with Obstruction: Consider Oncologic Resection vs Temporization with Delayed Elective Surgery
Treatment Approach
- Stage I-II: Resection
- T4b: Resect en Bloc with Portion of the Adjacent Organ
- Consider Adjuvant Chemo for High-Risk Stage II (Excluded if MSI-H or dMMR – Good Prognosis)
- Perforation or Obstruction
- T4 Lesion
- Indeterminate or Positive Margins
- Poorly Differentiated/Undifferentiated
- Lymphovascular or Perineural Invasion
- Non-Oncologic Resection (< 12 LN)
- Stage III: Resection & Adjuvant Chemo
- Stage IV:
- Resectable (Isolated Lung/Liver) – Resection & Adjuvant Chemo
- Consider Neoadjuvant Chemo
- Isolated Peritoneal Mets: Controversial
- Unresectable – Definitive Chemotherapy with/without Immunotherapy
- Asymptomatic: Avoid Surgery
- Symptomatic: Consider Palliative Resection, Stenting or Diverting Ostomy
- *Resect if Downstaged to Resectable
- Resectable (Isolated Lung/Liver) – Resection & Adjuvant Chemo
- *Consider Neoadjuvant Chemotherapy for:
- Clinical T4b Lesions
- Bulky Nodal Disease
- Metastases
Colon Resection
- Bowel Prep: Mechanical & Oral ABX
- Lower Rates of Surgical Site Infections, Anastomotic Leaks, Length of Stay & Readmission
- Resection
- Laparoscopic/MIS Preferred if Able
- Extent:
- Margin: 5 cm
- Complete Mesocolic Excision
- Remove Tumor En Bloc with Mesocolon & Regional Lymphadenectomy
- Resect Mesentery Back to the Primary Vessel Origin
- Oncologic Resection Requires: 12 Lymph Nodes
- Appendix – Right Hemicolectomy Indications:
- Appendix Adenocarcinoma (No Matter Size)
- Appendix Mucinous Tumor If:
- Moderate-Poor Differentiation
- Not Completely Resected
- Ruptured
- *Well Differentiated, Not Ruptured & Completely Resected are Debated – It Appears that NOT Preforming a Completion Right Hemicolectomy Has Similar Survival with Low Rates of Lymph Node Involvement
- Carcinoid Tumor
Chemotherapy Regimens
- FOLFOX – Leucovorin (Folinic Acid), 5-FU (Fluorouracil) & Oxaliplatin
- CAPEOX – Capecitabine & Oxaliplatin
- Other Regimens (Category 2B):
- FOLFIRI – Leucovorin (Folinic Acid), 5-FU (Fluorouracil) & Irinotecan
- FOLFOXIRI – FOLFOX + Irinotecan
Immunotherapy Options
- Bevacizumab (Avastin) – Vascular Endothelial Growth Factor (VEGF) Monoclonal Ab
- Cetuximab – Epidermal Growth Factor Receptor (EGFR) Monoclonal Ab
- Panitumumab – Epidermal Growth Factor Receptor (EGFR) Monoclonal Ab
Radiation Therapy (XRT)
- None in Colon CA – Risk Damage to Surrounding Viscera
- May Be Used in Rectal CA
Mnemonics
Criteria that Endoscopic Excision is Sufficient for Colon Cancer
- #2 Stools: Size < T2 & Margin > 2 mm
References
- Yamauchi T, Shida D, Tanizawa T, Inada K. Anastomotic Recurrence of Sigmoid Colon Cancer over Five Years after Surgery. Case Rep Gastroenterol. 2013 Oct 17;7(3):462-6.(License: CC BY-NC-3.0)
- Samir at English Wikipedia. Wikimedia Commons. (License: CC BY-SA-3.0)