Stomach: Gastrectomy
Antrectomy (Distal Gastrectomy)
Antrectomy (Distal Gastrectomy)
- Goals:
- Goal for CA: R0 Resection
- Margins: *See Stomach: Adenocarcinoma
- Goal for PUD: To Remove All G Cells Requires
- Requires ≥ 35% of Distal Stomach Removed
- About 45% of Lesser Curvature or 7 cm from Pylorus
- About 15% of Greater Curvature
- Goal for CA: R0 Resection
- Procedure:
- Preform a Kocher Maneuver to Minimize Tension
- Mobilize the Greater Curvature
- Ligate the Right Gastroepiploic Artery at the Pylorus
- Continue Dissection Around the Greater Curvature to the Extent Required for Reconstruction
- Mobilize the Lesser Curvature
- Divide the Lesser Omentum from the Incisura to the Pylorus
- Ligate the Right Gastric Artery at the Pylorus
- Resect Antrum & Pylorus as Appropriate
- Preform Selected Reconstruction
Antrectomy Reconstructions
- Billroth I
- Gastroduodenal Anastomosis
- Procedure: Stomach Remnant is Connected Directly to the Remaining Duodenum in a Continuous Fashion
- Comparison:
- More Anatomic than Billroth II
- Risk for Increased Tension
- Billroth II
- Gastrojejunal Anastomosis
- Procedure: Stomach Remnant is Connected Distally to the Jejunum Creating an Afferent Limb
- Limbs:
- Afferent Limb: Proximal Duodenojejunal Limb
- Efferent Limb: Common Distal Jejunal Limb
- Comparison:
- Overall More Complications Than Billroth I
- Highest Risk of Blind Loop Syndrome
- Roux-en-Y
- Procedure:
- Jejunum is Divided 40 cm Distal to the Ligament of Treitz
- Jejunojejunostomy is Made
- The Proximal End is Set 50-70 cm Down the Distal End
- A Side-to-Side Anastomosis is Made
- Gastrojejunostomy is Made
- The New Roux Limb is Anastomosed to the Stomach
- All Mesentery Defects are Closed
- Limbs:
- Roux Limb: Continuous Limb in Continuity with Stomach
- Biliopancreatic Limb
- Comparison:
- Less Dumping Syndrome
- Less Alkaline Reflux Gastritis
- Higher Risk of Marginal Ulcers
- Procedure:
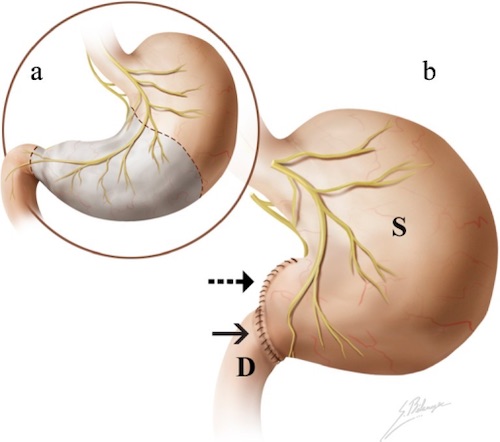
Billroth I 1
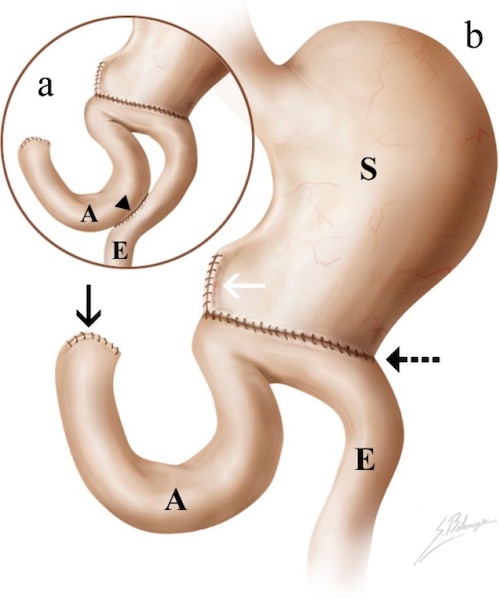
Billroth II 1
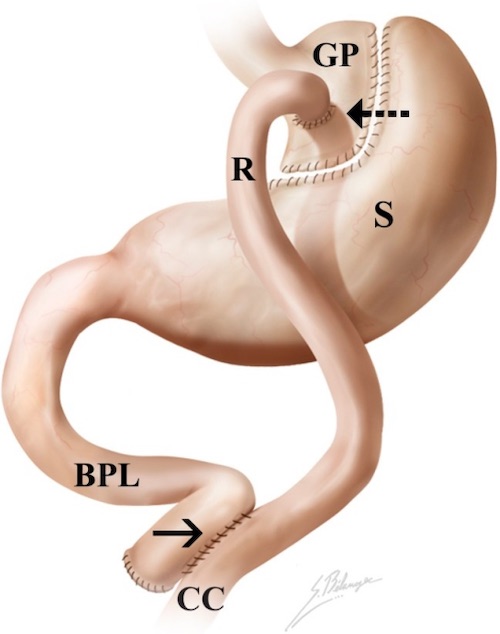
Roux-en-Y 1
Total Gastrectomy & D2 Lymphadenectomy
Total Gastrectomy & D2 Lymphadenectomy
- First Divide Hepatoduodenal Ligament to Visualize the Right Crus
- Divide Gastrocolic Ligament & Short Gastric Vessels
- Include Greater Curvature Lymph Nodes (Station 4) in Specimen
- Retract Stomach Up & Divide the Left Gastric Artery
- Preform a D2 Lymphadenectomy
- Start from the Proximal Common Hepatic (Station 8) & Continue to the Left Gastric Pedicle (Station 7)
- Continue Posteriorly to Celiac Node (Station 9) & Along the Splenic Artery (Station 11)
- Consider Inclusion of Splenic Hilum (Station 10) with Splenectomy
- Return Stomach to Natural Position
- Continue Dissection from Common Hepatic to the Anterior Hepatoduodenal Ligament to Include Hepatic Artery Nodes (Station 12a)
- Divide the Lesser Omentum Along the Lesser Curvature
- Include Lesser Curvature Lymph Nodes (Station 3) in Specimen
- Extend Hiatal Dissection from Right Crus to the Left Crus both Anteriorly & Posteriorly
- Include Pericardial Lymph Nodes (Stations 1-2) in Specimen
- Dissect the Proximal Duodenum to Include Pyloric Lymph Nodes (Stations 5-6)
- Resection
- Transect Duodenum 1-2 cm Distal to Pylorus
- Transect the Distal Esophagus
- Send Both Margins for Frozen Section
- Proceed with Greater Omentectomy
- Reconstruction of Choice Once Frozen Section Found Negative
Total Gastrectomy Reconstructions
- Roux-en-Y Esophagojejunostomy
- Classic Roux-en-Y with a Straight Jejunal Roux Limb
- Roux-en-Y with Jejunal J-Pouch (Hunt-Lawrence)
- Procedure:
- Jejunum is Divided 20-40 cm Distal to the Ligament of Treitz
- Distal End is Folded onto Itself and Formed into a Jejunal J-Pouch of 10 cm
- Jejunojejunostomy is Made with Proximal End Set 40-50 cm Down the Distal End
- Esophagojejunostomy is Made Anvil Circular Stapler from Esophagus to the J-Pouch
- Pouch Allows Prolonged Retention of Food
- Outcomes
- Best Outcomes
- Best Nutrition & Weight Gain
- Better Quality of Life
- Lower Risk of Esophagitis, Heartburn & Dumping Syndromes
- Procedure:
- Roux-en-Y with Looped Esophagojejunostomy
- End Esophagus to Side of Jejunum with a Small Blind End
- Jejunal Interposition
- Segment of Jejunum Resected and Interposed Between Esophagus & Proximal Duodenum
- Colon Interposition
- Segment of Colon Resected and Interposed Between Esophagus & Proximal Duodenum
- Double Tract
- Jejunum Transected & Distal Limb is Anastomosed to the Esophagus Similar to Roux-en-Y
- The Distal End of the Proximal Limb is Anastomosed About 40-50 cm Down the Roux Limb
- The Proximal End of the Proximal Limb is Anastomosed About 15-30 cm Down the Roux Limb Creating a Second Tract
Complications & Postgastrectomy Syndromes
Malnutrition
- Weight Loss is Common and Can Be Significant
- Anemia – Iron, Folate & B12
- Iron is the Most Common Vitamin Deficiency (Absorbed in Duodenum)
- Osteoporosis – Calcium
Gastric Emptying
- Dumping Syndrome
- Delayed Gastric Emptying
- From Chronic Atony
- *See Stomach: Gastric Emptying Diseases
Billroth II Obstructions
- Afferent Loop Obstruction
- Pathogenesis:
- Afferent Loop is Obstructed Causing Accumulation of Pancreatic/Hepatobiliary Secretions with Severe Epigastric Pain
- High Intraluminal Pressure Eventually Overcomes Positional Obstruction & Forces Fluid into the Stomach
- Causes High-Volume Bilious Vomiting & Relief of Symptoms
- Most Common Cause: Redundant Antecolic Afferent Limb (> 30-40 cm)
- More at Risk for Kinking, Volvulus and Adhesions
- Blind-Loop Syndrome (Also Known as Afferent Loop Syndrome)
- Tx: Surgery (Conversion to Roux-en-Y)
- Pathogenesis:
- Efferent Loop Obstruction
- Sx: Abdominal Pain, Distention & Bilious Vomiting
- Dx: Upper GI Contrast Study
- Tx: Balloon Dilation
- Surgery if Needed
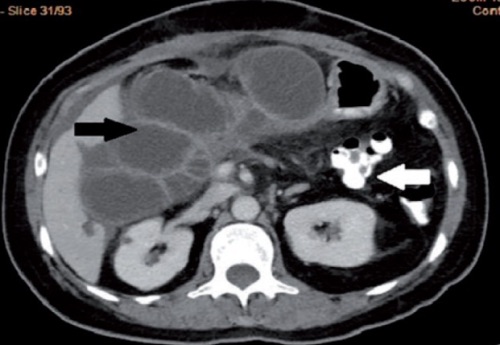
Afferent Loop Obstruction; Dilated Proximal Bowel (Black Arrow), Normal Distal Bowel (White Arrow) 2
Alkaline (Bile) Reflux Gastritis
- Bile Reflux into Stomach When Pylorus Unable to Prevent
- Histologic Bile Gastritis is Common but Clinical Bile Gastritis with Symptoms are Uncommon
- Most Common After Billroth II
- Sx: Abdominal Pain & Bilious Vomiting
- Pain Does NOT Resolve After Emesis (Compared to Afferent Loop Syndrome)
- Dx: HIDA
- Tx: Conservative (PPI, Reglan/Metoclopramide & Cholestyramine)
- If Fails: Conversion to Roux-en-Y Gastrojejunostomy
- Keep Roux Limb > 40 cm, Around 60 cm
- If Fails: Conversion to Roux-en-Y Gastrojejunostomy
Marginal Ulcers
- Ulcers that Develop at the Gastrojejunal Anastomosis
- Can Be on Either Side of the Anastomosis
- More Common After Roux-en-Y (Lacks the Buffering Afferent Limb Contents to Counteract Acid in Jejunal Mucosa)
- Retained Antrum Syndrome
- Recurrent Ulcer After Billroth II from Inadequate Removal of the Distal Antrum/Pylorus
- Retained Antral G Cells are Not Exposed to Luminal Acid Causing Increased Gastrin Secretion & Intense Acid Secretion in the Proximal Remnant & Marginal Ulcers
- Risk Factors:
- Ischemia
- H. pylori
- Gastrogastric Fistula
- Smoking
- NSAIDs
- Advise All Patient to Avoid Smoking & NSAIDs
- Tx: PPI & H. pylori Tx
- If Fails: Surgery

Marginal Ulcer of GJ Anastomosis 3
Duodenal Stump Blowout (Postgastrectomy Duodenal Leak)
- Causes:
- Poor Surgical Technique
- Inadequate Closure
- Devascularization
- Pancreatitis
- Afferent Obstruction
- Tx: Decompressive Duodenostomy Tubes & Drains
References
- Terrone DG, Lepanto L, Billiard JS, Olivié D, Murphy-Lavallée J, Vandenbroucke F, Tang A. A primer to common major gastrointestinal post-surgical anatomy on CT-a pictorial review. Insights Imaging. 2011 Dec;2(6):631-638. (License: CC BY-2.0)
- Chhabra P, Singh Rana S, Sharma V, Sharma R, Gupta R, Kumar Bhasin D. An unusual cause of simultaneous common bile and pancreatic duct dilation. Gastroenterol Rep (Oxf). 2015 Aug;3(3):258-61. (License: CC BY-3.0)
- Adduci AJ, Phillips CH, Harvin H. Prospective diagnosis of marginal ulceration following Roux-en-Y gastric bypass with computed tomography. Radiol Case Rep. 2016 Feb 17;10(2):1063. (License: CC BY-NC-ND-4.0)