Liver: Benign Mass & Cyst
Cystic Mass
Simple Cysts
- Benign
- Sx: Abdominal Pain & Nausea
- Mostly Small & ASx
- Most Common in Women
- Most Common in Right Lobe
- CT Findings:
- *See Liver: Mass CT Characteristics
- Well-Demarcated
- No Enhancement
- No Visible Wall
- Tx:
- ASx: Observation, No Serial Imaging
- Sx: Laparoscopic Wide Unroofing
- Percutaneous Aspiration Previously Recommended Now Found to Be Ineffective
Polycystic Liver Disease
- Causes:
- Associated with Polycystic Kidney Disease (Most Common)
- Autosomal Dominant Polycystic Liver Disease
- Autosomal Dominant
- Not Associated with PCKD or Cerebral Aneurysms
- Sx: Abdominal Pain & Nausea
- Mostly Small & ASx
- Tx:
- ASx: Observation
- Sx: Laparoscopic Wide Unroofing
- Avoid Estrogen
Noninvasive Mucinous Cystic Neoplasm (MCN)/Cystadenoma
- Most Common in Women
- Potential for Malignant Transformation
- Tx: Enucleation
- If Carcinoma Suspected: Liver Resection
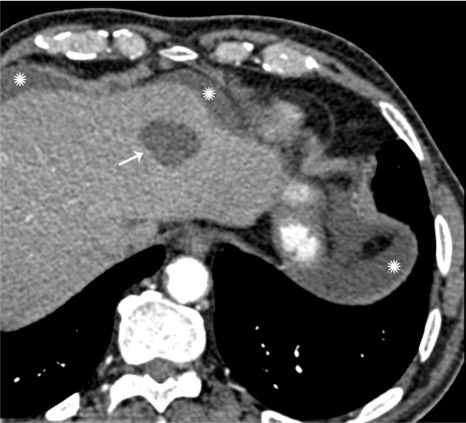
Simple Cyst of the Liver 1
Bile Duct Hamartoma (von Meyenburg Complex)
Basics
- Small (0.1-1.5 cm) White Lesion in Liver Periphery
- Benign with No Malignant Potential
- Often Associated with Polycystic Liver or Kidney Disease
- Most Common Liver Lesion Seen Incidentally in Laparotomy
- Tx: None
Hepatic Hemangioma
Basics
- Congenital Vascular Malformations that Enlarge by Ectasia
- Most Common Benign Liver Lesion
- Most Common in Adult Women
- Increase in Size During Pregnancy or With Estrogen Therapy
- Most Common in Right Lobe
- Mostly ASx
CT Findings
- *See Liver: Mass CT Characteristics
- Arterial Phase: Peripheral Enhancement
- Portal Venous Phase: Centripetal Flow
- Delayed Phase: Isodense Then Hypodense
- MRI:
- Smooth, Well-Demarcated & Homogenous
- Low Signal Intensity on T1
- Peripheral Nodular Enhancement
Treatment
- ASx: Conservative
- If > 5 cm: Repeat Imaging at 6-12 Months
- Sx: Enucleation or Liver Resection
- If Bleeding or Giant (> 10 cm): Preoperative Transarterial Embolization
Pediatric Considerations
- Most Common in Association with Multiple Skin Hemangiomas
- May Cause AV Shunting & CHF
- Kasabach-Merritt Syndrome: Consumptive Coagulopathy with Thrombocytopenia
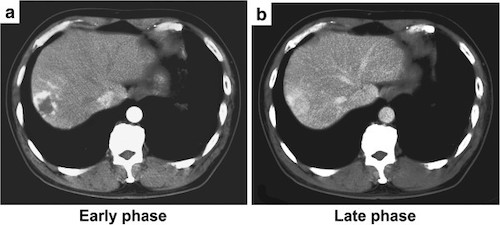
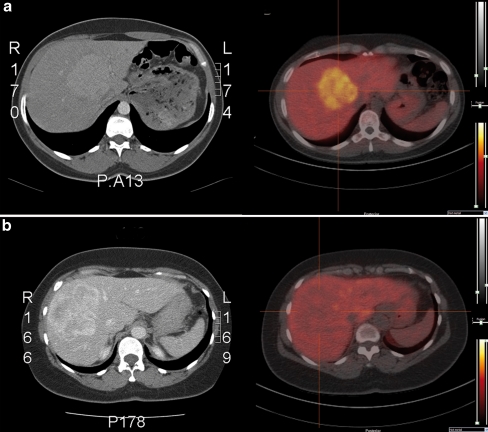
Hepatic Hemangioma. (a) Early Arterial Peripheral Enhancement, (b) Late Homogenous Attenuation 2
Focal Nodular Hyperplasia (FNH)
Basics
- Hyperplastic Hepatocytes Surrounding a Central Stellate Scar
- Cause: Disturbance in Blood Flow
- Most Common in Liver Periphery
- Second Most Common Benign Liver Lesion
- Most Common in Adult Women Although Estrogen is Not a Risk Factor
- Has Kupffer Cells – Takes Up Sulfur Colloid on Liver Scan
- Mostly ASx
Diagnosis
- Primarily on Imaging
- If Uncertain on Imaging: Bx
CT Findings
- *See Liver: Mass CT Characteristics
- Arterial Phase: Homogenous Enhancement
- Portal Venous Phase: Precontrast Density
- Central Stellate Scar
- Liver Scan: Hot
Treatment
- Primary Tx: Conservative
- If Persistent Sx: Resection
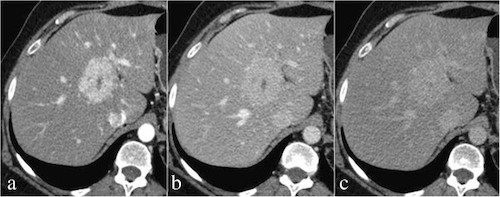
FNH. (a) Early Arterial Homogenous Enhancement with Central Scar, (b) Portal Venous Washout, (c) Delayed Phase Isodensity 3
Hepatocellular Adenoma (Hepatic Adenoma)
Basics
- Benign Epithelial Tumor
- Small Risk of Malignant Transformation
- Different from a “Hepatoma” – Hepatoma is Carcinoma
- Most Common in Adult Women
- Most Common in Right Lobe
- No Kupffer Cells – Does Not Take Up Sulfur Colloid on Liver Scan
- Most (75%) are Symptomatic (Abdominal Pain Most Common)
- Risk for Rupture, Particularly if > 5 cm
- No Bx (Bleeding Risk)
Risk Factors
- Majority Associated with Oral Contraceptive Pills
- Glycogen Storage Diseases
- Obesity
- Anabolic Steroids
CT Findings
- *See Liver: Mass CT Characteristics
- Well Circumscribed
- Variable Attenuation Depending on Calcification, Hemorrhage (Hyperattenuating) or Fat Content (Hypoattenuating)
- Similar to FNH
- Arterial Phase: Homogenous Enhancement
- Portal Venous Phase: Precontrast Density
- Liver Scan: Cold
Treatment
- Primary Tx: Stop Oral Contraceptive Pills & Weight Loss
- ASx & ≤ 5 cm: Repeat Imaging in 6 Months
- Sx or > 5 cm: Resection
- If Unresectable: Transarterial Embolization
- If Ruptured: Emergent Resection (Consider Preoperative Embolization)
- If Male: Resect All (Higher Risk of Malignant Transformation)
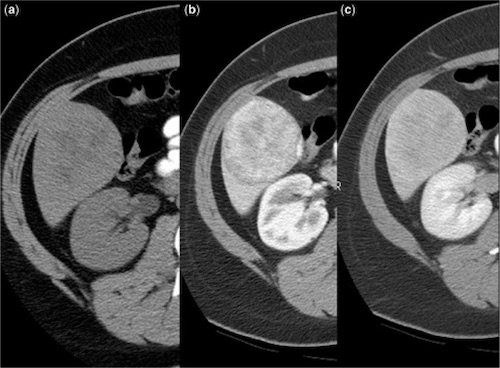
Hepatic Adenoma. (a) Precontrast, (b) Enhancement on Arterial Phase, (c) Gradual Washout on Delayed Phase 4
Liver Scan. (a) FNH (Hot), (b) HCA (Cold) 5
References
- Lazoura O, Vassiou K, Kanavou T, Vlychou M, Arvanitis DL, Fezoulidis IV. Incidental non-cardiac findings of a coronary angiography with a 128-slice multi-detector CT scanner: should we only concentrate on the heart? Korean J Radiol. 2010 Jan-Feb;11(1):60-8. (License: CC BY-NC-3.0)
- Shimada Y, Takahashi Y, Iguchi H, Yamazaki H, Tsunoda H, Watanabe M, Oda M, Yokomori H. A hepatic sclerosed hemangioma with significant morphological change over a period of 10 years: a case report. J Med Case Rep. 2013 May 28;7:139. (License: CC BY-2.0)
- Scialpi M, Pierotti L, Gravante S, Piscioli I, Pusiol T, Schiavone R, D’Andrea A. Split-bolus versus triphasic multidetector-row computed tomography technique in the diagnosis of hepatic focal nodular hyperplasia: a case report. J Med Case Rep. 2014 Dec 14;8:425. (License: CC BY-4.0)
- Gore RM, Thakrar KH, Wenzke DR, Newmark GM, Mehta UK, Berlin JW. That liver lesion on MDCT in the oncology patient: is it important? Cancer Imaging. 2012 Sep 28;12(2):373-84.(License: CC BY-4.0)
- van den Esschert JW, Bieze M, Beuers UH, van Gulik TM, Bennink RJ. Differentiation of hepatocellular adenoma and focal nodular hyperplasia using 18F-fluorocholine PET/CT. Eur J Nucl Med Mol Imaging. 2011 Mar;38(3):436-40. (License: CC BY-NC-2.0)