Liver: Cancer
Hepatocellular Carcinoma (HCC/Hepatoma)
Basics
- 4th Most Common CA-Related Death in the World
- Blood Supply Mostly from Hepatic Artery
- Most Common Site of Metastasis: Lung
Risk Factors
- HBV (Most Common Cause)
- Chronic HCV
- Cirrhosis (90% Have Chronic Liver Disease)
- Hereditary Hemochromatosis
- Male Gender
- Tobacco & Alcohol
- *No Increased Risk: Hepatitis A or Hormonal Therapy
Presentation
- Many are Asymptomatic
- Abdominal Pain
- Weight Loss
- Palpable Mass
Histology Subtypes
- Fibrolamellar (FLC)
- Best Prognosis
- Most Common in Peds
- Central Scar (Like FNH)
- Elevated Neurotensin & Normal AFP
- Steatohepatic – Resemble Steatohepatitis
- Clear Cell
- Macrotrabecular Massive
- Scirrhous
- Chromophobe
- Neutrophil Rich
- Lymphocyte Rich
Diagnosis
- Screening in HBV/Cirrhosis: US & AFP (Correlates with Size)
- Lesion < 1 cm: Repeat US & AFP Every 3-6 mo
- Lesion ≥ 1 cm: CT/MRI
- LI-RADS (Liver Imaging Reporting and Data System)
- LR-1: Definitely Benign
- LR-2: Probably Benign
- LR-3: Intermediate Probability of Malignancy
- LR-4: Probably HCC
- LR-5: Definitely HCC
- LR-M: Probably/Definitely Malignant
- Dx:
- LR-1/2: Routine Surveillance
- LR-3: Repeat Imaging in 3-6 Months
- LR-4: Follow-Up Imaging or May Require Bx
- LR-5: Tx (No Bx Needed)
- LR-M: Evaluate Underlying Malignancy, May Require Bx
CT Findings
- *See Liver: Mass CT Characteristics
- Arterial Phase: Early Enhancement
- Portal Venous/Delayed Phase: Washout
- Liver Scan: Cold
Hepatic Biopsy
- Percutaneous Biopsy (Preferred/Least Invasive)
- Absolute Contraindications:
- Uncooperative
- Significant Coagulopathy
- Significant Thrombocytopenia
- NSAIDs or Aspirin within 7-10 Days
- Refusal to Accept Blood Products
- Suspected Hemangioma or Echinococcal Cyst
- Unable to Identify Adequate Site
- Relative Contraindications:
- Morbid Obesity
- Ascites
- Amyloidosis
- Hemophilia
- Absolute Contraindications:
- Laparoscopic Biopsy
- Contraindications:
- Unable to Tolerate Pneumoperitoneum
- Hostile Abdomen
- Bowel Obstruction
- Bacterial Peritonitis
- Contraindications:
- Open Biopsy
Treatment
- No Cirrhosis or Child’s Class A: Resection
- Consider Portal Vein Embolization (PVE) if Functional Liver Remnant Too Small
- With Cirrhosis (Child’s Class B/C): Liver TXP
- Milan Criteria to Consider TXP in HCC:
- x1 Lesion ≤ 5 cm
- x3 Lesions All ≤ 3 cm
- No Gross Vascular Invasion
- No LN/Mets
- UCSF Criteria to Consider TXP in HCC:
- x1 Lesion < 6.5 cm
- x3 Lesions All < 4.5 cm with Total < 8.5 cm
- Less Commonly Used
- If Not TXP Candidate:
- Child’s Class C: Palliative Care
- Mets: Chemotherapy
- First-Line: Sorafenib #1 or Lenvatinib (Tyrosine Kinase Inhibitors)
- Second-Line: Regorafenib or Nivolumab
- No Mets: Locoregional Liver-Directed Therapy
- Options:
- Transarterial Chemoembolization (TACE)
- Radiofrequency Ablation (RFA)
- Microwave Ablation
- Stereotactic Body Radiation Therapy (SBRT)
- If Fails: Chemotherapy
- Options:
- Milan Criteria to Consider TXP in HCC:
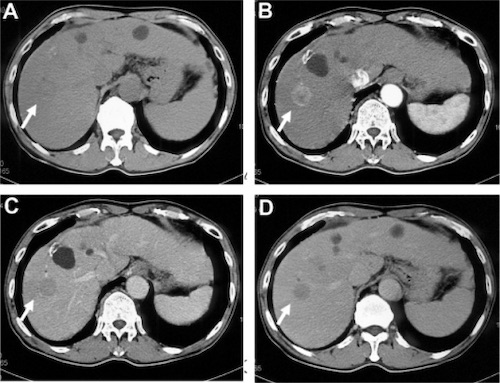
Hepatocellular Carcinoma. (a) Noncontrast, (b) Arterial Phase Enhancement, (c) Portal Phase Washout, (d) Delayed Phase Hypoattenuation 1
HCC TNM Staging – AJCC 8
- TNM
| T | N | M | |
| 1 | A – Solitary ≤ 2 cm
B – Solitary > 2 cm Without Vascular Invasion |
Any LN | Any Mets |
| 2 | Solitary with Vascular Invasion
Multiple < 5 cm |
||
| 3 | Multiple, At Least One > 5 cm | ||
| 4 | Invade Adjacent Organs or Major Hepatic/Portal Branch |
- Stage
| T | N | M | ||
| I | A | T1a | N0 | M0 |
| B | T1b | N0 | M0 | |
| II | T2 | N0 | M0 | |
| III | A | T3 | N0 | M0 |
| B | T4 | N0 | M0 | |
| IV | A | Any T | N1 | M0 |
| B | Any T | Any N | M1 | |
Metastases
Basics
- 20x More Common Than Primary Tumors
- Hypovascular (Primary Liver Tumors are Hypervascular)
- Derive Blood Supply from Hepatic Artery
- Most Sensitive Dx: Intraoperative US
Best Prognosis Indications
- ≤ 5 cm Size
- No Serosal Invasion
- Lymph Node Negative
- Fewer Metastases
- Metachronous > 1 Year from Resection of Primary (Disease-Free Interval Better)
- CEA < 200
CT Findings
- *See Liver: Mass CT Characteristics
- Arterial Phase: No Enhancement
- Some Such as NET, RCC, etc. May Have Rapid Enhancement
Treatment (If Liver-Isolated)
- Synchronous Lesions:
- Simultaneous Resection
- Resect Primary & Liver Lesions in Same Operations
- Resect Liver Lesion First, Then Primary Lesion
- Require Fluid Restriction to Keep CVP Low During Liver Resection
- Can Fluid Resuscitate Once Liver Resection Done
- Preferred by Patients
- Indication:
- ASx Primary in Favorable Location (Right Colon) & Limited Metastases
- Resect Primary & Liver Lesions in Same Operations
- “Classic” Two-Stage Resection
- Resect Primary Colorectal Lesion First, Then Resect Liver Lesion at Later Procedure
- Indications:
- Symptomatic Primary Lesion
- Extensive Bilobar Disease – Likely to Require Portal Vein Embolization
- Difficult Primary Location
- Elderly > 70 Years Unlikely to Tolerate Extended Operation
- “Reverse” Two-Stage Resection
- Resect Liver Lesion First, Then Resect Primary at Later Procedure
- Indications:
- Locally Advanced Primary Cancer Requiring Neoadjuvant Chemotherapy
- Simultaneous Resection
- Metachronous Lesions: Resection
- Consider Portal Vein Embolization if Functional Liver Remnant Too Small
- Chemotherapy – Regimen & Timing Controversial
- If Patient Receives Neoadjuvant Chemotherapy & Restaging Shows Complete Response: Still Preform a Hepatic Resection (Complete Response is Rare)
- TXP Never Indicated
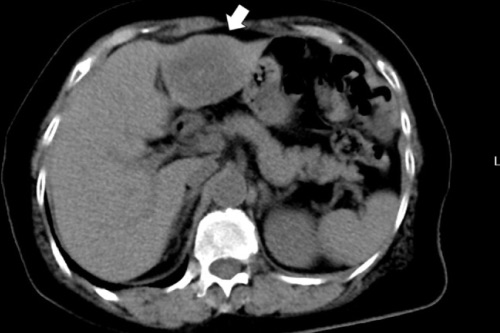
Liver Metastasis from Colon Cancer 2
Other Malignant Mass
Mucinous Cystic Neoplasm with Associated Invasive Carcinoma/Cystadenocarcinoma
- MCN with Malignant Change in the Inner Epithelial Lining
- Tx: Liver Resection
Hepatoblastoma
Hepatic Angiosarcoma
- High-Grade Vascular Malignancy
- Most Common in Elderly Men
- Associated with Vinyl Chloride, Arsenic or Anabolic Steroid Exposure
- Sx: Abdominal Pain, Fatigue & Weight Loss
- Risk for Budd-Chiari Syndrome or Bleeding
Hepatic Epithelioid Hemangioendothelioma (EHE)
- Low-Grade Vascular Malignancy
- High Rate or Metastasis
- Most Common in Adult Women
- Sx: Abdominal Pain, Fatigue & Weight Loss
- Risk for Budd-Chiari Syndrome
Cholangiocarcinoma
References
- Murakami T, Tsurusaki M, Hyodo T, Imai Y. Clinical utility of imaging for evaluation of hepatocellular carcinoma. J Hepatocell Carcinoma. 2014 Jul 14;1:101-8. (License: CC BY-NC-3.0)
- Ito T, Kushida T, Sakurada M, Maekawa H, Orita H, Mizuguchi K, Sato K. Two cases of laparoscopic simultaneous resection of colorectal cancer and synchronous liver metastases in elderly patients. Int J Surg Case Rep. 2016;26:134-7. (License: CC BY-NC-ND-4.0)