Large Intestine: Ulcerative Colitis (UC)
Ulcerative Colitis (UC)
Basics
- Inflammatory Bowel Disease (IBD) – Chronic Inflammatory Disease of the Colonic Mucosal Layer
- Associated with HLA B27
- Also Ankylosing Spondylitis & Sacroiliitis
- Smoking is Not a Risk Factor & May Actually Be Protective
- Increased Risk of Malignancy Starting 8-10 Years After Disease Onset
- Surgery is Curative
Inflammation
- Continuous Inflammation from the Rectum Proximally
- Spares the Anus
- Inflammation Confined to the Mucosa/Submucosa
- Most Common Site of Perforation: Transverse Colon
Presentation
- Symptoms:
- Diarrhea – Most Common Symptom
- Bloody Stools
- Abdominal Pain
- Tenesmus (Feeling of a Frequent Need to Defecate Even if Already Passed a Bowel Movement)
- Fecal Incontinence
- Complications:
- GI Bleed
- Stricture
- Backwash Ileitis
- Toxic Colitis
- Toxic Megacolon
- Perforation
- Fulminant Ulcerative Colitis
- Definition: ≥ 10 Bloody Stools Daily, Often with Pain & Distention
- A Subset of Severe Ulcerative Colitis
Extraintestinal Manifestations
- Arthritis – Most Common Extraintestinal Manifestation
- Ankylosing Spondylitis
- Uveitis or Episcleritis
- Rash – Erythema Nodosum or Pyoderma Gangrenosum
- Primary Sclerosing Cholangitis
- Venous Thromboembolism
Diagnosis
- Dx: Based on Presence of Chronic Diarrhea ≥ 4 Weeks & Evidence of Chronic Colitis oin Endoscopy
- Must Exclude Other Similar Causes
- Testing:
- Imaging (CT or MRI)
- “Lead Pipe” Appearance of the Colon on Abdominal XR
- “Collar Button Ulcers” from Undermining at the Lateral Ulcer Edges
- Colonoscopy with Intubation of Terminal Ileum & Mucosal Bx
- Imaging (CT or MRI)
- Morphology:
- Mucosal Edema (Earliest Sign)
- Friable Mucosa – Causes Bleeding
- Polymorphonuclear Cells in Lamina Propria
- Crypt Abscess
- Mucosal Ulceration
- Pseudopolyps of Surrounding Mucosa
Montreal Classification
- Extent
- E1: Ulcerative Proctitis: Confined to Rectum
- E2: Left-Sided/Distal Ulcerative Colitis: Distal to Splenic Flexure
- E3: Extensive Ulcerative Colitis/Pancolitis: Extends Proximal to the Splenic Flexure
- Severity
- S0: Clinical Remission: Asymptomatic
- S1: Mild: ≤ 4 Stools Daily with No Systemic Illness & Normal ESR
- S2: Moderate: > 4 Stools Daily with Minimal Signs of Toxicity
- S3: Severe: ≥ 6 Bloody Stools Daily & ≥ 1 Sign of Systemic Toxicity
- Signs: Pulse Rate ≥ 90, Temperature ≥ 37.5 C, Hgb < 10.5 g/dL or ESR ≥ 30 mm/h
Mayo Scoring System
- Scores 0-12 Indicate Disease Severity & Should Be Used to Compare to Previous Patient Scores
- Stool Pattern:
- 0: Normal Number of Stools
- 1: 1-2 More Stools Than Normal
- 2: 3-4 More Stools Than Normal
- 3: ≥ 5 More Stools Than Normal
- Most Severe Rectal Bleeding of the Day:
- 0: None
- 1: Bloody Streaks ≤ Half the Time
- 2: Blood in Most Stools
- 3: Pure Blood Passed
- Endoscopic Findings:
- 0: Inactive: Normal
- 1: Mild: Erythema, Decreased Vascular Pattern or Mild Friability
- 2: Moderate: Marked Erythema, Absent Vascular Pattern, Friability or Erosions
- 3: Severe: Spontaneous Bleeding or Ulceration
- Global Physician Assessment:
- 0: Normal
- 1: Mild Colitis
- 2: Moderate Colitis
- 3: Severe Colitis
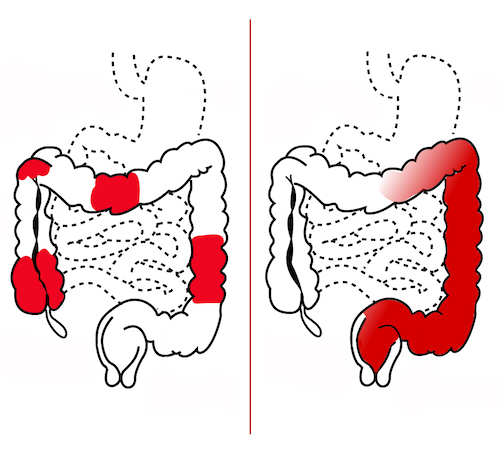
Skip Lesions of Crohn’s (Left) Compared to Continuous Lesion of UC (Right) 1

“Lead Pipe” Sigmoid Colon on XR 1
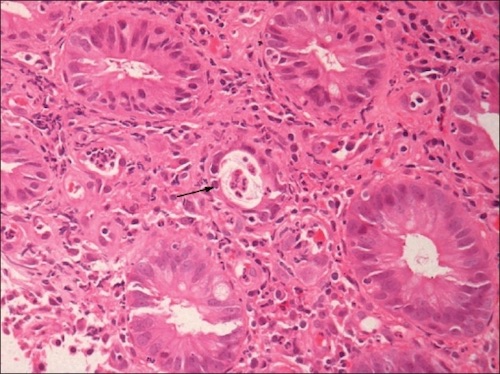
Crypt Abscess 3

Pseudopolyps 4
Ulcerative Colitis (UC) – Treatment
Medical Treatment
- Acute Flares/Fulminant Colitis: Steroids and/or Biologics
- Biologics:
- Infliximab (Remicade) – TNF-α Inhibitor
- Adalimumab (Humira) – TNF-α Inhibitor
- Golimumab – TNF-α Inhibitor
- Vedolizumab – Anti-Integrin Ab
- Tofacitinib – Janus Kinase Inhibitor (Increased Risk of VTE – Second Line)
- Infection Control: Cipro/Flagyl
- Biologics:
- Maintenance: 5-Aminosalicylic Acid (Sulfasalazine/Mesalamine)
- Oral and/or Rectal (Topical/Suppository/Enema)
Management of Dysplasia
- Definitions:
- Visible – Found on a Targeted Biopsy of a Visible Lesion
- Invisible – Found on Random Biopsy with No Visible Lesion
- Visible Dysplasia:
- Completely Excised: Continue Endoscopic Surveillance
- Not Completely Excised: Proctocolectomy
- If There is Any Invisible Dysplasia in the Surrounding Flat Mucosa: Proctocolectomy
- Invisible Dysplasia: Repeat Colonoscopy in 3-6 Months by an Experienced Endoscopist
- Should Be High-Definition with Chromoendoscopy (Uses Optic Filters or Contrasts/Dye Agents to Better Differentiate Abnormal Mucosa)
- Indications for Total Proctocolectomy After Repeat Exam:
- Invisible Multifocal Low-Grade Dysplasia
- Invisible High-Grade Dysplasia
- *Historically ANY Dysplasia was an Indication for Total Proctocolectomy – Changed in ASCRS 2021 Recommendations
Surgery Indications
- Emergent Surgery:
- Refractory Fulminant Colitis
- Perforation
- Massive GI Bleed
- Toxic Megacolon
- Elective Surgery:
- Medical Intractability (Not Tolerated or Getting Worse) – Most Common Indication
- Obstruction
- Malignancy
- Failure to Thrive in Children – Most Common Extraintestinal Indication
Surgical Treatment
- Emergent: Total Abdominal Colectomy & End Ileostomy
- Open if Megacolon Present
- Second Stage Completion Proctectomy & Ileal Pouch Anal Anastomosis When Stabilized
- Elective: Total Proctocolectomy & Ileal Pouch Anal Anastomosis
- IPAA Will Have ≥ 5-6 BM’s Daily
- Indications for End Ileostomy:
- Poor Sphincter Function
- Poor Mobility
- Lifestyle/Occupation Not Permitting Frequent BM’s
- Malnourished or Immunocompromised
- May Be Completed in Stages:
- One-Stage
- 1. Total Proctocolectomy & IPAA (No Ostomy)
- Two-Stage
- 1. Total Proctocolectomy, IPAA & Loop Ileostomy
- 2. Ileotomy Takedown
- Three-Stage
- 1. Subtotal Colectomy & End Ileostomy
- 2. Proctectomy, IPAA & Loop Ileostomy
- 3. Ileostomy Takedown
- One-Stage
- Protect Bladder/Sexual Function
- Need Lifetime Surveillance
- Most Common Complication: Leak
Extraintestinal Manifestations After Colectomy
- Manifestations that Improve:
- Erythema Nodosum
- Arthritis
- Eye Problems
- Manifestations that Improve for Some (50%):
- Pyoderma Gangrenosum
- Manifestations that Do Not Improve:
- Primary Sclerosing Cholangitis
- Ankylosing Spondylitis
Inflammatory Bowel Disease (IBD) Comparison
Chrohn’s Disease
Inflammatory Bowel Disease Type Unspecified
Comparison
References
- Wikimedia Commons. (License: CC BY-4.0)
- Norsa AH, Tonolini M, Ippolito S, Bianco R. Water enema multidetector CT technique and imaging of diverticulitis and chronic inflammatory bowel diseases. Insights Imaging. 2013 Jun;4(3):309-20. (License: CC BY-4.0)
- Parameswaran S, Singh K, Nada R, Rathi M, Kohli H, Jha V, Gupta K, Sakhuja V. Ulcerative colitis after renal transplantation: A case report and review of literature. Indian J Nephrol. 2011 Apr;21(2):120-2. (License: CC BY-NC-SA-3.0)
- Haggstrom M. Wikimedia Commons. (License: CC0 1.0)